This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
Ectopic gastric mucosal structures are largely considered asymptomatic or relatively unimportant. Recently, more and more symptoms have been reported to be associated with these esophageal lesions, making them a subject of controversy.
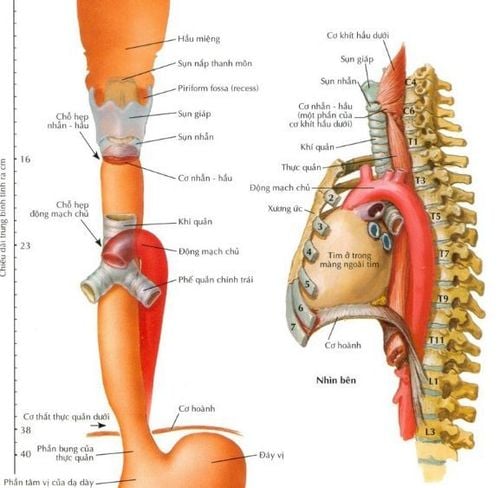
1. What is the esophagus? Where is the esophagus located?
The esophagus is the first part of the digestive tube that carries food from the pharynx to the stomach, about 25cm long, relatively mobile, attached to the surrounding organs by loose, flattened structures because the walls are close to it. each other and have a tubular shape when swallowing food. The esophagus is connected to the pharynx at the level of the 6th cervical vertebrae, below the gastric outlet at the cardia, at the level of the 10th thoracic vertebra. The esophagus is located posterior to the trachea, descends to the posterior mediastinum, is located posteriorly. heart and anterior to the thoracic aorta, through the diaphragm into the abdomen, to the stomach.
2. Structure of the esophagus
Anatomically, the esophagus is about 25 cm long and at its narrowest point is about 1.5 cm in diameter divided into 3 segments: cervical; thorax and abdomen. The lumen of the esophagus also has three narrow places: the junction with the pharynx at the level of the cricoid cartilage; at the level of the left aorta and left main bronchus; heart hole.
Neck segment: about 3cm long, food will run through the trachea and then to 1/3 of the neck, the food will shift to the left and down to run parallel to the trachea and then continue through the inlet behind the chest to enter the chest segment. Chest segment: about 20cm long, food entering the chest will continue through the diaphragm to enter the abdomen. Abdominal segment: about 2cm long, food has reached the abdomen, then through the foramen into the stomach.
3. What is ectopic gastric mucosa in the esophagus?
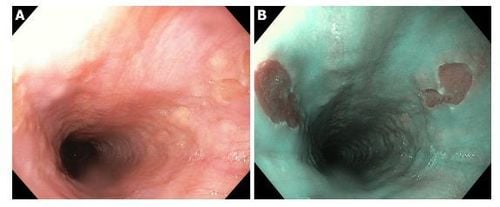
Ectopic gastric mucosa structures (ectopic gastric mucosa structures) are an area of surrounding mucosa that is salmon-pink in color, variable in size and oval, round or even with map shape. It is often observed during endoscopic evaluation of the cervical esophagus. Ectopic gastric mucosal structures may have a smooth surface or a slightly raised or concave surface with regular or irregular borders. Rarely, ectopic gastric mucosal structures may present as a convex lesion or multiple polyps. Small lesions may be covered by squamous epithelium and present without obvious changes in the upper esophageal mucosa.
4. Current situation of diagnosis of this pathology
Ectopic gastric mucosal structures are largely considered asymptomatic or relatively unimportant. Recently, more and more symptoms have been reported to be associated with these esophageal lesions, making them a subject of controversy. Currently, there are no standard guidelines for the management of ectopic gastric mucosal symptoms of the esophagus. In particular, the diagnosis of the condition through the use of a longer extubation time combined with the routine use of optical endoscopy in the esophagus may be useful to further explore the significance of these structures. misplaced gastric mucosa.
5. Ectopic gastric mucosal structure and accompanying non-neoplastic lesions
The association of ectopic gastric mucosal structure with Barrett's esophagus and gastric lesions such as Helicobacter pylori-associated gastritis (H. Pylori) has been debated in many studies.
5.1 Ectopic gastric mucosa and Barrett's esophagus Conflicting results regarding the association between ectopic gastric mucosa and Barrett's esophagus indicate that their interaction is largely speculative. However, a genetic link between Barrett's esophagus and ectopic gastric mucosal structures can be disputed due to their immunohistochemical similarities, including expression of the same mucin core protein. and their cytokeratin patterns.
In contrast, Feurle et al. evaluation of neuroendocrine immunohistochemical staining patterns of ectopic gastric mucosa and Barrett's esophagus revealed that they are distinct parts of an anterior differential spectrum. , with ectopic gastric mucosal structures representing the embryonic stage of gastric mucosa, while cells from Barrett's esophagus represent more primitive and pluripotent cells.
5.2 H. pylori and ectopic gastric mucosa There is also controversy surrounding the suspected association of H. pylori with ectopic gastric mucosa and reflux esophagitis. Some authors have hypothesized that reflux may be required for H. pylori to colonize ectopic gastric mucosal structures.
However, there are differences in the literature in conclusions regarding the correlation between H. Pylori and the incidence of gastroesophageal reflux disease (GERD). Other studies have hypothesized that dyspepsia, including the sensation of choking, is caused by chronic inflammation produced by H. pylori in the gastric mucosa of ectopic gastric mucosal structures. One specific case report showed that eradication of H. pylori could ameliorate extragastric symptoms associated with ectopic gastric mucosal structures and lead to beneficial histopathological changes, which This study suggests that H. pylori and H. pylori eradication therapy may have different effects in patients with ectopic gastric mucosal structures. However, this report was limited by the fact that the patient had both H. pylori bacteria in the stomach and esophagus. Therefore, it was not possible to determine whether the improvement in swallowing sensation and heartburn was due solely to eradication of H. pylori. or proton pump inhibitors (PPIs) are often included in treatment.
The oxyntic mucosal cell type is the most commonly reported, but the cardiac, antral and mixed (both oxyntic and antral) cell types have also been detected. Ectopic gastric mucosa of ectopic gastric mucosal structures is highly susceptible to H. pylori infection, with an incidence of up to 82%. However, this high percentage can be questioned if we consider that the gastric H. pylori detection is thought to occur in the antrum type mucosa.
5.3 . Ectopic gastric mucosa and pathogenicity of H.Pylori In contrast, another study showed that the type of gastric mucosa ectopic gastric mucosa did not affect the rate of H. pylori invasion and detection. found that H. pylori density and mucosal type were the only predictors of active inflammation in ectopic gastric mucosal structures and were more likely to be inflamed in H. PYLORI-infected patients active in the mucosa other than those of the ectopic gastric mucosal structure.
In 2010, Alagozlu et al found that ectopic gastric mucosal structures were positive for H. pylori in 23.5% of patients with a higher localization rate in female patients than in male patients ( P < 0.05), and further showed that the sensation of choking is a symptom persistence. Interestingly, this study found that H. pylori was most prevalent in the muscular mucosa (81.2%) and that synchronous H. pylori I gastritis was present in all patients with structural infections ectopic gastric mucosal structure. Size ranges have been reported, from 5 to 32 mm and from 10% to 30% of the circumference of the proximal esophagus, but they did not determine whether the increased localization rate was size dependent.
5.4 Size of ectopic gastric mucosa and association with clinical symptom severity However, some reports have shown that size of ectopic gastric mucosa may be related to symptoms ( eg, correlation with dysphagia severity) and hypothesized that it may be a function of increased acid secretion or narrow scar formation at the distal end of ectopic gastric mucosal structures.
The majority of studies have found a correlation between the prevalence of H. pylori in ectopic gastric mucosal structures and their gastric density, which suggests that invasion cannot be performed. Independent occupation of ectopic gastric mucosal structures. However, isolated infiltration of ectopic gastric mucosal structures has also recently been described without the involvement of H. pylori-positive gastritis.
Fortunately, a 5-year follow-up of 20 patients with both ectopic gastric mucosa in the cervical esophagus and H. pylori infection by Latos et al did not find any malignant changes, dysplasia, or metaplasia. any. However, their study was likely limited by a small number of patients.
A retrospective analysis of a larger population showed a significant association between ectopic gastric mucosal structure and male sex, sensation of choking, dysphagia, upper respiratory tract complaints, Barrett's esophagus and Barrett's esophagus. Interestingly, there was no association between abnormal gastric mucosal structure and dysplasia or adenocarcinoma in women.
6. Conclusion
Ectopic gastric mucosal structural entities are subject to being ignored, unexplored, and become a source of curiosity. Its natural history and clinical significance are still poorly defined due to the limited number of ambiguous studies in the literature. Unfortunately, the role of esophageal ectopic gastric mucosa in various symptoms is still poorly understood and is mainly based on speculation, while gender-related prevalence remains to be seen. calculate.
The authors recommend frequent and careful cervical esophageal examination to develop the differential diagnosis, especially in patients with initial functional dyspepsia and those with upper dysphagia, cough, and dysphagia. Chronic unexplained or persistent sensitivity. The malignancy of ectopic gastric mucosal structures and its association with other entities such as Barrett's esophagus remains controversial.
>> See more: Treatment and screening for ectopic gastric mucosa in the esophagus - Posted by Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Raine CH . Ectopic gastric mucosa in the upper esophagus as a cause of dysphagia. Ann Otol Rhinol Laryngol . 1983; 92 :65-66. [PubMed] [DOI] Truong LD, Stroehlein JR, McKechnie JC. Gastric heterotopia of the proximal esophagus: a report of four cases detected by endoscopy and review of literature. Am J Gastroenterol . 1986; 81:1162-1166. [PubMed] Akbayir N , Alkim C, Erdem L, Sökmen HM, Sungun A, Başak T, Turgut S, Mungan Z. Heterotopic gastric mucosa in the cervical esophagus (inlet patch): endoscopic prevalence, histological and clinical characteristics. J Gastroenterol Hepatol . 2004; 19:891-896. [PubMed] [DOI] Borhan-Manesh F , Farnum JB. Incidence of heterotopic gastric mucosa in the upper oesophagus. Gut . 1991; 32 :968-972. [PubMed] [DOI] Tang P , McKinley MJ, Sporrer M, Kahn E. Inlet patch: prevalence, histologic type, and association with esophagitis, Barrett esophagus, and antritis. Arch Pathol Lab Med . 2004; 128 :444-447. [PubMed] [DOI] Adriana Ciocalteu, Petrica Popa, Issues and controversies in esophageal inlet patch, World J Gastroenterol. Aug 14, 2019; 25(30): 4061-4073