This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
A classification system for sphincteric dysfunction as a structural abnormality was established in 1988. Originally called the Hogan-Geenan classification of sphincteric dysfunction, it was later revised to the Milwaukee classification. intended to classify patients with sphincter dysfunction into categories 1, 2, and 3 based on clinical presentation as well as laboratory or imaging abnormalities.
1. What is oddi sphincter dysfunction?
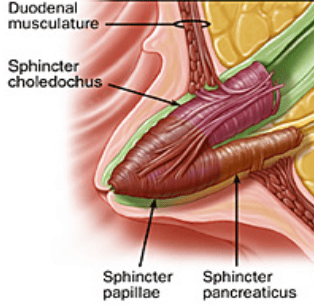
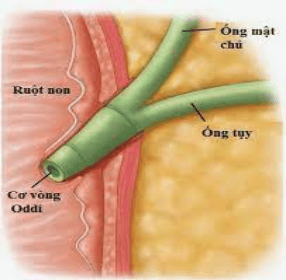
Sphincter of Oddi dysfunction is a clinical syndrome caused by dyskinesia of the sphincter of Oddi (functional) or anatomical (mechanical) obstruction associated with abdominal pain and elevated liver or pancreatic enzymes; dilation of the common bile duct, pancreatic duct, or pancreatitis.
The term sphincter disorder of Oddi more specifically denotes disorders of the sphincter of Oddi movement, while sphincter dysfunction includes both mechanical obstruction and dyskinesia of the sphincter of Oddi. Since the advent of scintigraphy, gallbladder dysfunction is now recognized as a discrete entity and should be differentiated from sphincter of Oddi dyskinesia.
Different forms of primary sphincteric dysfunction are considered functional gastrointestinal disorders and can occur in adults or children of any age, but sphincteric dysfunction is most common in women aged 20–50 years. The estimated prevalence of sphincter dysfunction is 1.5% in the general population and may be as high as 72% in patients with idiopathic recurrent acute pancreatitis based on small cohort studies. . However, its true prevalence is difficult to determine due to the lack of biomarkers or definitive diagnostic criteria as well as the multitude of secondary causes of sphincter dysfunction, such as fibrosis. channel sphincter (papillary stenosis and sclerotic papillary sclerosis) or obstructive carcinoma.
2. Clinical manifestations of sphincter dysfunction
Sphincter of Oddi dysfunction may involve the biliary sphincter, the pancreatic sphincter, or both. Biliary sphincter dysfunction usually presents with recurrent biliary pain, characterized by epigastric or right upper quadrant pain lasting 30 minutes to several hours with or without elevation of liver enzymes.
Pain may radiate to the back, shoulder or shoulder blades and may be accompanied by nausea and vomiting. Pain is intermittent after eating and is not relieved by changing positions, taking antacids, or having a bowel movement.
Disorders of the pancreatic sphincter are thought to be responsible for a fraction of patients with recurrent episodes of acute pancreatitis. The patient will have pain in the mid-abdomen, in the pancreas, radiating to the back, associated with increased serum amylase and lipase. Symptoms related to the pancreatic sphincter are often aggravated by ingestion. No other cause of pancreatitis is commonly found in these patients and they can be classified as having idiopathic recurrent acute pancreatitis (IARP).
3. Classification of sphincter disorders oddi
Diagnosis of sphincter dysfunction is challenging, but history, physical examination, relevant routine histopathology tests, and imaging studies are important. Some view sphincter dysfunction as a structural abnormality, while others view it as a dysfunction.
A classification system for sphincteric dysfunction as a structural abnormality was established in 1988. Originally called the Hogan-Geenan classification of sphincteric dysfunction and later revised to the Milwaukee classification , it classifies patients with sphincter dysfunction into categories 1, 2, and 3 based on clinical presentation as well as laboratory and/or imaging abnormalities. These criteria are intended to make diagnostic evaluation more applicable to clinical practice and, whenever possible, avoid invasive procedures by emphasizing noninvasive imaging of the bile duct diameters. owner.
Previous studies have shown higher rates of depression, obsessive-compulsive disorder, and anxiety in patients with type 3 sphincter dysfunction when compared with controls. In contrast, a randomized, controlled trial of patients with type 3 sphincter dysfunction found psychosocial disability in patients with severe symptoms that may not differ from the general population.
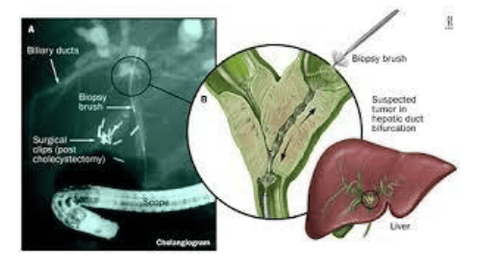
3.1. Milwaukee classification for biliary sphincter dysfunction Type 1: Biliary colic associated with all three of the following: Serum aminotransferases >2 times the limit of normal; Common bile duct dilatation ≥ 10 mm on ultrasound or 12 mm on ERCP; Slow drainage (>45 min) of contrast from the common bile duct on ERCP. Type 2: Biliary colic associated with one or two of the following: Serum aminotransferases >2 times the limit of normal or common bile duct dilatation ≥ 10 mm for ultrasound or 12 mm for ERCP and slow drainage (>45 min) of contrast from the common bile duct on ERCP. Type 3: Only biliary colic only. 3.2. Milwaukee classification for pancreatic sphincter dysfunction Type 1: Pancreatic pain associated with all three of the following: Serum amylase or lipase >2 times the limit of normal; Dilation of the pancreatic duct (pancreatic duct) > 6 mm in the head of the pancreas and > 5 mm in the body of the pancreas; Slow drainage (>9 min) of contrast agent from the pancreatic duct on ERCP. Type 2: Pancreatic pain associated with one or two of the following: Serum amylase or lipase >2 times the limit of normal or pancreatic ductal dilation >6 mm in the head of the pancreas and >5 mm in the body of the pancreas or slow drainage (>9 min) of contrast from the pancreatic duct on ERCP. Type 3: Pancreatic pain only.
3.3. Rome III classification of sphincter dysfunction Pain in the right epigastric or upper abdomen is associated with ≥1 of the following:
Duration ≥30 minutes Recurrent symptoms occur at intervals variable duration (not daily) Occurs more than 1 time in the last 12 months Pain gradually increases to a stable level Moderate to severe pain sufficient to disrupt daily activities No evidence of structural abnormality
4. Other evaluations for sphincter dysfunction
Previously, noninvasive testing for the diagnosis of sphincter disorders included quantitative hepatobiliary scintigraphy to assess bile flow, endoscopic ultrasonography, or magnetic resonance cholangiography with secrettin injection. However, these tests are not sensitive and not specific for sphincter dysfunction.
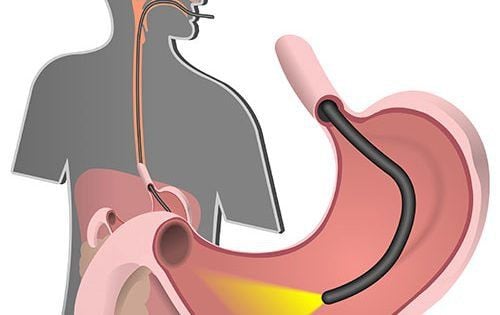
The sphincter of Oddi measurement is considered the gold standard test for diagnosing sphincter dysfunction. During sphincter of Oddi manometry, a catheter is inserted into the duodenum and corrected to 0 mmHg. Next, the catheter is inserted into the common bile duct and/or pancreatic duct for 30 seconds; A baseline pressure ≥ 40 mmHg indicates sphincter dysfunction. Prior to the procedure, patients should avoid agents that inhibit sphincter of Oddi function, such as anticholinergics, nitrates, calcium channel blockers, and minor stimulants such as opiates and cholinergics.
There are limitations to the measurement of the sphincter of Oddi, which are:
First, it requires a skilled endoscopist with special equipment not available in most institutions; Second, it is associated with up to a 30% increased risk of acute pancreatitis; Finally, the isolation-time pressure measurements obtained during the sphincter of Oddi manometer may not reflect the dynamic nature of the sphincter of Oddi, leading to difficulty in applying the results. Therefore, the use of the sphincter of Oddi manometer as the gold standard test remains controversial. Furthermore, isolated basal pressure cannot distinguish between sphincter of Oddi dyskinesia and anatomical stenosis. Of note, manometry is not conclusive in 13–40% of patients ultimately diagnosed with type 1 sphincter dysfunction.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Elham Afghanistan. Sphincter of Oddi Function and Risk Factors for Dysfunction. Front Nutr. Year 2017; 4: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5276812/