This is an automatically translated article.
The consequence of an immune system disorder is the formation of abnormal antibodies against antigens present on red blood cells. This disorder causes autoimmune hemolytic disease, which is also an autoimmune disease.
1. Causes of autoimmune hemolytic disease
1.1 Allogeneic immunity
Autoimmune hemolytic disease caused by allogeneic immune antibodies, common in some of the following cases:
Rh blood group incompatibility in newborns due to Rh-positive mothers while the child has Rh+ blood group, or according to the ABO system, the mother has blood type O and the child has blood type A. Due to a transfusion of "dangerous O" blood group, due to abnormally high anti-A or anti-B. Due to the wrong blood type, the ABO system is not suitable. Due to the abnormal formation of immune antibodies in the case, transfusion of non-blood subtypes, leukocyte antigens, platelets, and Rh. 1.2 Hemolytic anemia
Autoimmune hemolytic anemia or autoimmune hemolytic anemia as a result of stimulation by an animal or plant antigen that is chemically very similar to that of the red blood cell group, occurs in the following cases:
The state of increasing immunity by injecting a drug carrying antigens such as: vaccines containing antitoxins (anti-diphtheria, tetanus ...) because of these ingredients have A and B antigens. Use a number of therapeutic drugs made from animals (stomach essence, liver, anti-hemophilie components of pigs...). Immunization in volunteers with Witebiky for sample serum preparation. 1.3 Loss of normal inhibitory function of T-lymphocytes
The mechanism by which autoimmune hemolysis can occur is when T-lymphocytes lose their normal inhibitory function. When T lymphocytes due to a certain cause can no longer be tolerated, at this time, B lymphocytes will freely produce abnormal antibodies and are expressed through some of the following cases:
Mechanism Cross-reaction: When infected with streptococcus (Streptococcus) will cause anti-cardiac and anti-renal antibodies because Streptococcus has common antigens with the kidneys and heart. Streptococcus antigen-specific T lymphocytes take the place of cardiac and renal antigens, and the B lymphocytes are therefore uninhibited to produce autoantibodies. The antigenic mechanism is masked: During fetal development, there are some tissues without blood vessels that do not come into contact with the corresponding lymphocyte clones, so they are "not forbidden". If, because of an injury, that blood-less tissue enters the circulation, there will be a specific reaction against, for example, eye crystals, testicles... Role of the virus: Virus's own antigenic mechanism can be expressed on infected cell membranes and cause damage to lymphocytes by virus fusion into the cytoskeletal genome, leading to loss of normal T-lymphocyte function and malignancy. Therefore, autoimmune hemolytic anemia is also seen in some malignancies.

Cơ chế tan máu tự miễn co thể xảy ra là khi tế bào lympho T mất đi chức năng ức chế bình thường
2. Diagnosis of autoimmune hemolytic anemia
To diagnose autoimmune hemolytic anemia or autoimmune hemolytic anemia, your doctor may order some blood and urine tests. Based on the test results, the doctor will make an accurate diagnosis of the disease.
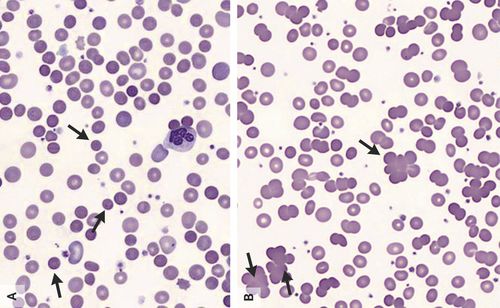
2.1 Whole blood test
Blood test results will show the indicators of components in the blood, including:
Hemoglobin is a protein that helps carry oxygen around in the body. The hematocrit indicates how much volume the red blood cells take up. If both of these numbers are low, it could be a sign of anemia.
2.2 Coombs test
Antibodies that affect red blood cells are found through the Coombs test.
2.3 Reticulocyte test
Reticulocytes are completely immature red blood cells. The number of reticulocytes present in the body reflects whether the bone marrow is making a normal number of red blood cells.
Red blood cell count may be higher if hemoglobin levels are low due to bleeding or destruction. Therefore, the body's increased production of red blood cells is likely a sign of anemia.
2.4 Bilirubin test
Yellow eyes and skin can be caused by the death of blood cells, hemoglobin is transferred into the blood and in turn broken down into bilirubin. High levels of bilirubin in the blood can be a sign of anemia, liver damage, or another medical condition.
2.5 Haptoglobin test
The liver makes a protein called Haptoglobin. In the body, they bind to a specific type of hemoglobin in the blood. Through the amount of haptoglobin in the blood will know how quickly red blood cells are being destroyed.
2.6 “Cold” Agglutinin Test
This type of autoimmune hemolysis associated with “cold” agglutinin is quite rare, symptoms often worsen when the body is exposed to low temperatures (range 0 - 10 degrees Celsius). ).
Agglutinin is an antibody that causes red blood cells to clump together. “Cold” antibodies work in cold temperatures, whereas “warm” antibodies work at normal body temperature. “Warm” antibodies may be present when:
Having certain infections such as mycoplasma pneumonia. Using several medications, including penicillin.

Bác sĩ có thể sẽ yêu cầu bệnh nhân tiến hành một số xét nghiệm máu
3. Is autoimmune hemolytic disease curable?
The doctor's choice of autoimmune hemolytic therapy for a patient depends on several factors. If the anemia is mild, it will usually clear up on its own without treatment. Approximately 70-80% of patients require no treatment or minimal intervention.
However, some people will need medication, surgery, or a blood transfusion.
Treatment using corticosteroids: The first dose is 1-2 mg/kg/day. The body responds well to the drug when the hemoglobin is > 80G/L, the dose is gradually reduced (30% of the dose/week). In case the patient has a life-threatening autoimmune hemolytic disease, the doctor may prescribe high-dose corticosteroids.
The doctor will base on each patient's drug response status to prescribe a maintenance dose to achieve a balance between the effectiveness and side effects of the drug. When the patient's hemoglobin returns to normal, the drug can be maintained at a dose of about 4mg / day, if within 1 year the disease does not recur, the drug can be stopped.
Use other immunosuppressive drugs in case the disease does not respond to corticosteroids such as: Azathioprine (Immurel), Cyclophosphamide, Cyclosporin A, Vincristin, Mycophenolate mofetil. Use Gamma globulin in emergency, hemolytic episodes, poor response to blood transfusion and corticosteroids. Splenectomy: This indication is given in cases where treatment with corticosteroids and immunosuppressants has failed for 3-6 months, or is dependent on high doses of corticosteroids. No other medical problems. Patient volunteers. Use of Rituximab: This is a B lymphocyte anti-CD20 monoclonal antibody, which reduces the production of anti-red blood cell antibodies. Indicated when immunosuppressive treatments and splenectomy are not effective. Other supportive treatment methods:
Blood transfusion Plasma exchange: Helps eliminate the maximum amount of antibodies circulating in the blood, reducing the clinical degree of hemolysis. Treatment and prevention of drug and disease complications. Some other treatment measures such as thymectomy, purine metabolism inhibitors (Cladribin) have been effective in some cases with persistent progression. If you need medical examination and treatment, you can go directly to Vinmec Health System nationwide, or contact to book an appointment online HERE.
MORE:
What is an autoimmune disease? What is autoimmune hemolytic disease? How is thalassemia (congenital hemolysis) treated?