This is an automatically translated article.
The article was written by MSc Vu Duy Dung - Doctor of Neurology, Department of General Internal Medicine - Vinmec Times City International HospitalSpinal cord arteriovenous fistula is often difficult to diagnose, but if detected in time, it will become easier to treat. Today's article will delve into the clinical aspects of the disease so that readers can fully understand the exact information of the disease, thereby having a timely treatment plan before the clinical manifestations worsen. .
1. Definition and Epidemiology
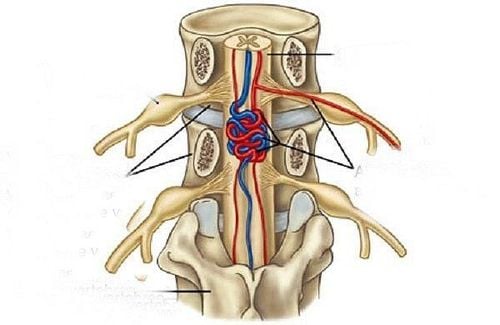
Spinal arteriovenous fistula is characterized by an abnormally direct connection between a root-bulb artery and a root-bulb vein without mediation of a capillary bed. The veins will become engorged and unable to drain in time for the inflow of blood, leading to increased venous pressure, and eventually infarction when parenchymal perfusion pressures drop to the point where adequate blood supply cannot function. cells when posterior venous pressure is greater than anterior arterial pressure. The site of the fistula itself is most common in the dura surrounding the nerve root in the intervertebral foramen. Arteriovenous fistula of the spinal cord is an acquired disease, but the etiology has not been found to date.
Arteriovenous fistula of the spinal cord is a rare disease; but they account for 60% to 80% of all spinal vascular malformations. They are mainly seen in men in their 60s and the most common site is the lower thoracic medulla.
2. Clinical manifestations
The symptoms that first appear in the setting of a dural arteriovenous fistula will be localized to the CSF and then ascend to the skull over time, because of venous congestion in the dural arteriovenous fistula. The spinal cord is preferentially transmitted posteriorly to the spinal cord. This ascent, coupled with the nonspecific nature of symptoms, may be reminiscent of a polyneuropathy or polyneuropathy. This condition is challenging to diagnose early and is often misdiagnosed. In fact, on average, diagnosis is delayed 1 to 3 years after symptom onset.
Sensory-motor symptoms are most common at first, and symptoms may be asymmetric early on, although they will later become symmetrical as the disease progresses. Sensory symptoms include numbness, paresthesia, back pain, or radicular pain. Numbness and decreased sensation may extend to the perianal area, and a degree of sensation is present in one-third of patients. Injury to the upper extremities does not occur other than in rare cases of cervical dural arteriovenous fistula.
Bowel, bladder, and sexual dysfunction often presents late. At diagnosis, up to 70% of patients will have a combination of upper and lower motor neuron signs.
The disease usually progresses slowly but can be gradual in one-third of patients and 5% of patients will present an acute episode without warning symptoms. Acute exacerbation with venous maneuvers such as exercise, prolonged standing, and the Valsalva maneuver is common. Approximately 50% of patients report clinical worsening of motor and sensory symptoms with intravenous methylprednisolone and no improvement after discontinuation of the drug.

Clinical features that can help distinguish dural arteriovenous fistula from other diagnoses:
Weakness and asymmetric sensory abnormalities Combination of upper and lower motor neuron signs Clinical worsening with Intravenous methylprednisolone Weakness worsened on exertion, prolonged standing, or singing No upper extremity signs/symptoms with ascending lower extremity signs/symptoms (ie, no glove-stocking distribution) Abnormal sensation of sacral skin segmentation With bowel/bladder symptoms without other features of a microfiber/vegetative neuropathy
3. Visual Features
Intensity on T1 and intramedullary T2 hyperintensity extending across 3 to 7 vertebral levels with peripheral preservation or a border of hypointensity on T2 (indicating deoxygenated hemoglobin) are characteristic. characteristic of spinal cord disease due to a dural arteriovenous fistula. Edema secondary to venous congestion may be present, but in severe cases the spinal cord may atrophy. Spinal cord disease is usually seen primarily in the cerebrospinal fluid and increased contrast enhancement may be present. Dilated and tortuous veins may be seen as flow voids on the ventral or dorsal surfaces of the spinal cord. Failure to see areas of flow and signal voids on spinal cord T2 on a full-axis spinal MRI would essentially rule out the diagnosis of a spinal arteriovenous fistula.
Catheter angiography remains the gold standard for the diagnosis of dural arteriovenous fistula and plays a key role in determining the method and therapeutic approach with structural and site information. leak. Magnetic contrast-enhanced magnetic resonance angiography (MRA) can accurately locate dural arteriovenous fistula in about 80% of cases by showing early venous filling at the site of the fistula. and can be used before routine angiography to allow for selective contrast injection and to minimize exposure to radiation and iodine.

4. Differential diagnosis
Arteriovenous fistulas are often misdiagnosed at first as degenerative disc disease, transverse myelitis, Guillain-Barré syndrome, spinal stenosis, amyotrophic lateral sclerosis, and peripheral vascular disease. , or polyneuropathy. The cost of misdiagnosis can be high. A recent study found that 96% of patients with delayed diagnosis for an average of 6 months experienced clinical deterioration with 60% requiring a walker or wheelchair.
5. Treatment
Surgical or endovascular treatment options are available to disconnect the vein from the blood supply artery. Endovascular intervention for venous occlusion with liquid embolization is successful in about 70% of cases, can be performed on initial angiography, and helps reduce hospital stay relative to open surgery. However, patients with feeding arteries proximal to Adamkiewicz's artery or anterior spinal artery and a narrow space at the base of the target vessel requiring intervention may be at high risk for displacement-related spinal infarction. button material. In these cases, open dissection is often considered. The rate of recanalization is higher with embolization and patients should be monitored clinically and imaging if symptoms return.
Surgical dissection of venous drainage is considered more certain and successful in 98% of cases. This technique has a complication rate of 2% with experienced physicians and in large centers. A multimodal approach with a combination of embolization and surgery may be indicated in patients with complex dural arteriovenous fistula with multiple feeding vessels.

6. Prognosis
Regardless of treatment modality, nearly all treated patients experience clinical improvement or stability. Two-thirds of patients will have an improvement in gait and activities of daily living, while one-third will have an improvement in bladder symptoms 1 year after treatment. Improvement in sensory symptoms, including pain, was more variable, but at least not worse. The strongest predictors for favorable outcome after treatment were pre-treatment clinical severity and successful disconnection of the fistula site. However, even patients with the most severe clinical manifestations have a good chance of improving postoperatively, and symptom severity should not be a reason to refuse treatment.
Vinmec International General Hospital is a high-quality medical facility in Vietnam with a team of highly qualified medical professionals, well-trained, domestic and foreign, and experienced.
A system of modern and advanced medical equipment, possessing many of the best machines in the world, helping to detect many difficult and dangerous diseases in a short time, supporting the diagnosis and treatment of doctors the most effective. The hospital space is designed according to 5-star hotel standards, giving patients comfort, friendliness and peace of mind.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: Kramer CL. Vascular Disorders of the Spinal Cord. Continuum (Minneap Minn) 2018;24(2, Spinal Cord Disorders): 407–426.