This article was consulted with Specialist Level I Doctor Le Thanh An - Interventional Cardiologist - Outpatient Department and Internal Medicine Department - The Vinmec Nha Trang International General Hospital.
Theoretically, a coronary stent (or coronary metal scaffold) will last as long as the person who receives it. In recent years, medical device companies have been creating biodegradable stents (scaffolds), meaning these stents will degrade and disappear a couple of years after placement. However, there is still a lack of evidence regarding the efficacy and safety of these new devices.
Essentially, patients are concerned about how long the effectiveness of coronary stents will last. In other words, patients want their coronary arteries to remain open, without restenosis, and without the placement for another stent. This depends on each individual's constitution, lifestyle habits, a healthy diet, regular exercise, and the need to take medication as prescribed by the doctor.
1. What is a coronary stent?
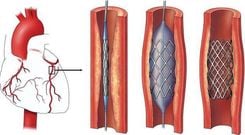
A coronary stent is a small mesh tube made of metal or polymer, with or without a drug coating, that is used as a scaffold inside a coronary artery to prevent it from blockage or narrowing.
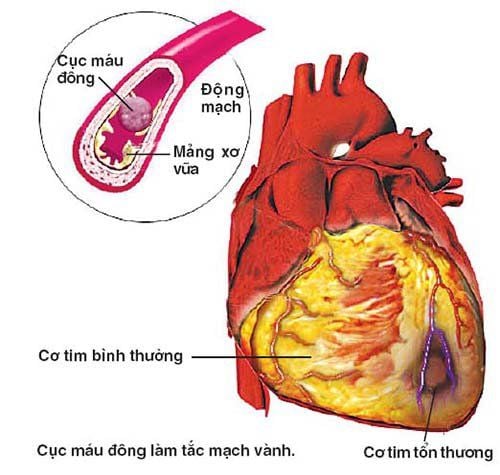
Coronary stent placement is a minimally invasive procedure that involves inserting a balloon and stent into a narrowed coronary artery to expand the artery and allow blood to flow to the ischemic heart muscle. This helps prevent heart attacks or minimize the area of heart damage, allowing patients to resume their activities without experiencing chest pain.
2. Factors Influencing Stent lifespan
Coronary stents are made of metal, so they will remain permanently in the coronary artery (except for biodegradable stents, which dissolve after 2 years).
If we look at it from a different perspective, we can say that the lifespan of a stent is the duration of its long-term effectiveness. Typically, a stent can stabilize the coronary artery for a long time (10-15 years). However, if the patient and doctor do not properly control the factors that lead to hardening of the coronary arteries, this time can be reduced (to as little as a few months).
Risk factors that can lead to stent restenosis include smoking, high-fat diet, irregular medication, uncontrolled diabetes, high blood pressure or lipid level disorders, incomplete stent coverage of the lesion, sedentary lifestyle, etc.
It is important to emphasize that smoking is the leading cause of stent restenosis. In the first period of time after stent placement, patients need to take dual antiplatelet therapy (Aspirin combined with Clopidogrel or Ticagrelor/Prasugrel). Since the stent is a foreign object in the body, if dual antiplatelet therapy is not used, platelets and red blood cells will stick to the stent and form a blood clot, which is a very dangerous complication with a high mortality rate. Therefore, patients must adhere to the medication as prescribed by their doctor.
Factors related to the stent placement process that reduce the lifespan of the stent:
● Increased proliferation of the vascular media: the process of balloon dilation and stent placement affects the vascular media, stimulating its proliferation and covering the inside of the stent, leading to stent narrowing after a few months or even several years.
● Neointimal hyperplasia: new atherosclerotic plaques will form inside the stent, causing stent restenosis. This occurs due to unhealthy lifestyle habits, inappropriate diet and exercise, poor adherence to treatment, or due to the patient's own constitution.
Moreover, the risk of restenosis increases with the number of stents placed.
3. Types of coronary stents
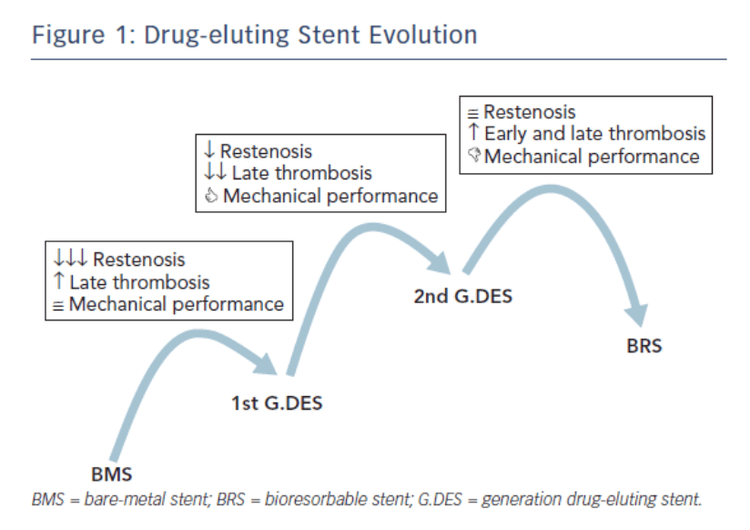
Bare metal stents (BMS) and drug-eluting stents (DES) are commonly used. Additionally, there are newer generation stents being developed to address the Disadvantages of earlier stents.
3.1. Bare Metal Stent (BMS)
This is the first-generation coronary stent, made from bare metal (usually stainless steel) and without a special coating. The restenosis rate after placement of this stent is 17-41%.
3.2. Drug-Eluting Stent (DES)
This type of stent has a metal frame similar to a bare metal stent but is coated with a drug that prevents restenosis within the stent, reducing the risk of restenosis to below 10%.
3.3. Bioresorbable Scaffold (BRS)
This is a stent made from a special biodegradable scaffold (essentially poly-lactate, or desaminotyrosine polycarbonate, or magnesium), which can be completely absorbed by the body over time, allowing the coronary artery to restore its original natural status. Although recent research data shows that the restenosis rate of BRS is significantly lower than that of drug-eluting stents (only 2%), BRS has not been widely used due to an increased risk of stent thrombosis compared to current stents.
5. How to Care for and Prolong the Lifespan of a Stent in your Body?
Caring for a patient after coronary stent placement is important in prolonging the lifespan of the stent and the patient's life.
5.1. Medications for coronary stent placement patients
Antiplatelet and anticoagulant medications after stent placement are mandatory and must be adhered to.
In addition, people with other comorbidities such as dyslipidemia, hypertension, diabetes, heart failure, etc. also need to take specific medications.
5.2. Diet plays a key role
● Food for stent patients is a double-edged sword, it can contribute to prolonging the lifespan of the stent but can also increase the risk of restenosis.
● Eat more fiber, which reduces the absorption of fat and cleans the blood vessels. Fiber is abundant in vegetables, fruits, brown rice, and whole grains.
● Avoid stimulating beverages, coffee, soft drinks, or carbonated water, as they can increase the process of blood vessel damage. Drinking filtered water and green tea is much better.
● Say no to animal fats, not only in fat but also found in skin, offal, and dark red meat. This does not mean completely avoiding fat, as the body still needs this compound for many other activities. Supplement healthy fats with walnuts, almonds, peanuts, cashews, olive oil, sunflower oil, etc.
● Eat fish more often, at least 3 times a week. This is also a source of lean protein and omega-3 fatty acids, which are extremely beneficial for the heart and brain.
● Develop a habit of eating bland and low-sugar foods, which helps to limit high blood pressure and diabetes in heart patients.
5.3. Regular exercise is necessary
Note that after coronary stent placement, moderate exercise is still recommended. Exercise helps increase the heart's endurance and promotes blood circulation.
You can do any form of activity, starting gently with 30 minutes, then gradually increasing the level and intensity.
Brisk walking is ideal as it helps form a collateral circulation system, which are small capillaries in the area of the ischemic heart muscle. Therefore, the heart is better perfused.

5.4. Remember to avoid stress
Stress is one of the causes that damage blood vessels, allowing bad cholesterol, calcium, and metabolic waste to accumulate and form atherosclerotic plaques, narrowing the blood vessels.
It is best to take time to rest and relieve stress from work and life. If possible, you can practice meditation, yoga, and travel more.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.