Specialist Level II Doctor,
Nguyen Quoc Viet
This article is written by Dr. Nguyen Quoc Viet, a Level II Specialist in Interventional Cardiology, Department of Internal Medicine, Vinmec Danang International Hospital.
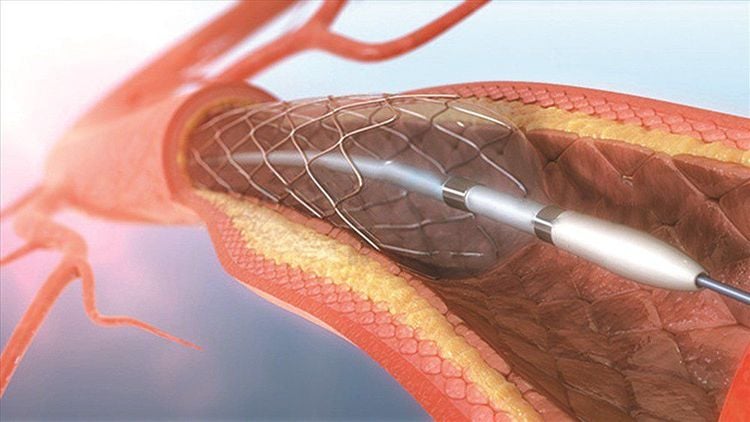
When one or more coronary arteries become narrowed or blocked, doctors perform percutaneous coronary intervention (PCI) with stent placement to restore blood flow. The procedure typically takes about an hour, and the patient remains awake under local anesthesia. After the procedure, patients can often be discharged within 1–2 days.
1. What is Coronary Stent Placement?
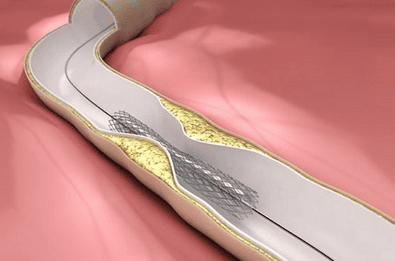
During the procedure, a doctor administers local anesthesia at the access point (either the radial or femoral artery) and inserts a guiding sheath. A catheter is advanced to the coronary artery, where the narrowed or blocked segment is located. A balloon catheter with a stent is guided to the site, where the balloon is inflated to expand the artery. The stent remains in place to maintain blood flow.
2. Who Should Undergo Coronary Stent Placement?
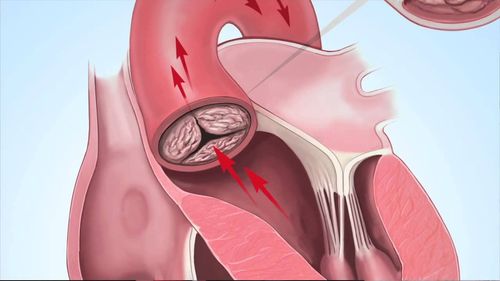
When atherosclerotic plaques narrow an artery by 50–70%, the coronary artery cannot supply adequate oxygen to the heart muscle, especially during physical exertion. This leads to ischemia, manifesting as chest pain or shortness of breath. A cardiologist will examine and recommend coronary angiography under fluoroscopy (DSA system). If the angiography results show severe narrowing or blockage, and the narrowing pattern is suitable, the doctor will recommend placing a coronary stent.
3. Post-Stent Care
Patients who undergo coronary stent placement must strictly follow their doctor’s instructions:
- Patients who have had a coronary stent placed need to take their medication fully and according to the prescribed regimen to ensure that no blood clots form, causing acute blockage in the stent in the early days, and to prevent the risk of restenosis at the stent site and reinfarction in the remaining coronary arteries. The patient should use long-term medication as directed by a cardiologist
- Smoking should be stopped because nicotine in cigarettes constricts blood vessels, damages the entire vascular system, increases the process of atherosclerosis, and causes narrowing within the stent and other coronary artery locations. Quitting smoking is the best way to reduce the risk of coronary artery disease events.
- Exercise after stent placement: Lifestyle changes are crucial in the treatment process. Exercise is essential and should follow the principle of starting slowly and gradually increasing to achieve an appropriate level of exertion.
- Diet is also an important factor in treatment: Foods beneficial for patients after coronary stent placement should be nutritious but not contain too much harmful fat. The total amount of fat consumed in a day should not exceed 25-35%. Harmful fats such as saturated fats, cholesterol (found in animal fat, skin, organs, red meat, egg yolks, shrimp…), and trans fats (found in packaged foods, fast food, and processed foods) should be limited. Increase beneficial fats, which are unsaturated fats found in olive oil, fish, and nuts like walnuts and almonds. These can help reduce blood LDL-c, lower blood pressure, limit atherosclerosis, and bring many benefits to coronary artery disease patients. Additionally, limit salt, carbohydrates (sugar, starch), and eat plenty of fiber and fresh fruits.
4. How long does a coronary stent last?
The lifespan of a coronary stent depends on its type. Coronary stents can exist permanently in the artery or bioresorbable stents dissolve over time.
The effectiveness of stents in preventing vascular blockage is temporary. Coronary artery blockage can continue to occur in other parts of the coronary system. Restenosis or acute blockage within the stent can happen if the patient does not adhere to the treatment regimen prescribed by the specialist.
Just because a coronary stent has been placed does not mean the patient is completely cured of coronary artery disease. Therefore, patients need to strictly follow the doctor’s instructions after stent placement.
5. How to reduce the risk of restenosis
To reduce the risk of restenosis after stent placement, patients should follow these post-stent guidelines:
- Take medications as prescribed by your doctor. Regularly take your medication and attend follow-up appointments at 1 month, 3 months, 6 months, and 1 year after stent placement.
- At the 1-year mark, have a follow-up examination and stress test to check the blood flow to your heart.
- Dietary Changes: Quit smoking and alcohol, lose weight if overweight, reduce intake of animal fats, fried foods, and limit salt.
- Eat plenty of vegetables and fruits.
- Regular Exercise: Patients should avoid strenuous physical activities.
- Instead, they should engage in light walking for 30-60 minutes each day. Gradually increase the intensity to improve physical fitness.
At Vinmec Da Nang International General Hospital, a team of specialists with many years of experience in various fields, along with comprehensive and modern specialized equipment, is available
- The Cathlab is equipped with state-of-the-art devices such as DSA machines, meeting the requirements for coronary artery imaging and interventions with the most minimally invasive techniques.
- The inpatient area features completely private rooms, fully equipped with supportive and convenient facilities.
- The clinic is also equipped with advanced cardiovascular diagnostic devices such as 2D and 3D echocardiography machines with full transesophageal and transthoracic ultrasound, ECG machines, blood pressure Holter monitors, ECG Holter monitors, and stress ECG machines.
- For consultation and treatment using coronary angiography, balloon angioplasty, and stent placement at Vinmec, you can contact 02363711111 or register HERE.