This is an automatically translated article.
The article was written by TS.BS Vu Hoang Huy - Emergency Doctor - Emergency Department - Vinmec Times City International General HospitalPulmonary embolism (PE) is when a blood clot (thrombus) breaks off and travels through your bloodstream to your lungs. If a blood clot blocks one or more blood vessels in your lungs, it's called a pulmonary embolism.
1. What is pulmonary embolism?
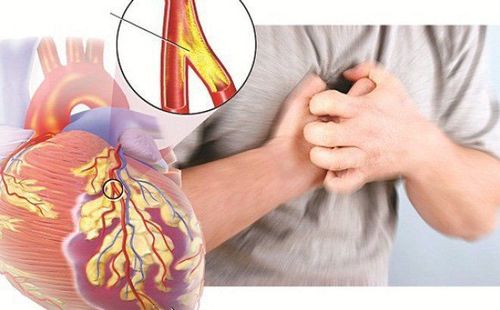
Pulmonary embolism usually arises from thrombosis originating in the deep venous system of the lower extremities; however, it also rarely originates in the pelvic veins, upper extremities, or the right heart chambers. After traveling to the lungs, large thrombus can lodge at the bifurcation of the main pulmonary artery or lobar branches and cause pulmonary and hemodynamic compromise.Pulmonary thromboembolism is not a local disease. Rather, it is a complication of primary venous thrombosis.
2. Pathophysiological mechanism of pulmonary embolism
PE occurs when a deep vein thrombosis dislodges and obstructs pulmonary circulation. Pulmonary embolism occurs and impairs gas exchange and circulation.Acute respiratory consequences of PE include:
Increased alveolar dead space Hypoxemia Hyperventilation The main cause of hypoxemia is 3 mechanisms as follows:
Inappropriate ventilation - perfusion. Obstruction of the pulmonary arteries produces dead space ventilation because alveolar ventilation exceeds pulmonary capillary blood flow. This contributes to ventilation-perfusion mismatch, with vascular occlusion of the arteries increasing pulmonary vascular resistance. In addition, humoral mediators, such as serotonin and thromboxane, are released from activated platelets and may cause vasoconstriction in unaffected lung areas. Areas of normal lung that are not infarcted are over-perfused, resulting in inadequate ventilation to provide oxygen to fully saturate the increased blood volume. Shunt occurs in the damaged lung area with collapsed and infarct, the lung is not ventilation but still has perfusion. In addition, shunts from the right atrium to the left atrium due to increased pressure in the right atrium. Mixed venous hyposaturation is caused by hypoxic hypoxic cardiac output. Hemodynamic consequences:
Pulmonary embolism reduces the cross-sectional area of the pulmonary vascular bed, leading to an increase in pulmonary vascular resistance, thereby increasing the right ventricular afterload. If right ventricular afterload increases severely, right ventricular failure may occur. In addition, humoral and reflex mechanisms contribute to pulmonary artery constriction. As the pulmonary artery systolic pressure increases, the right ventricular afterload will increase, leading to acute right ventricular failure. As right ventricular failure progresses, impaired left ventricular filling may develop. In addition, increased right ventricular pressure leads to RV dilatation. This can cause interventricular septal deviation, further reducing left ventricular diastolic filling. Rapid progression to myocardial ischemia may occur secondary to inadequate coronary artery filling, potentially with hypotension, syncope, electromyography dissociation, or sudden death.

3. When can pulmonary embolism cause death?
When more than 50% of pulmonary circulation is suddenly obstructed, the pathophysiology and clinical findings are dominated by severe cardiac and pulmonary dysfunction.The thin-walled right ventricle designed to resist normal pulmonary vascular resistance is low; it works poorly when suddenly clogged. As a result, it dilates and an increase in the systolic pressure of the right ventricle and pulmonary artery occurs, rarely exceeding 55 mmHg, because the right ventricle lacks time to develop compensatory hypertrophy, unable to generate output higher pressure.
Right ventricular end-diastolic pressure and right atrial pressure increase about 15–20 mmHg in RV failure. Right ventricular dilatation leads to tricuspid regurgitation and may compromise left ventricular filling.
Cardiac output is reduced and the patient is hypotensive. This can cause a sudden loss of consciousness. If the degree of obstruction is sufficient, death occurs almost immediately. Decreased aortic pressure and increased right ventricular pressure can cause right ventricular ischemia through severe right coronary hypoperfusion. Electromyography dissociation is the most common cause of eventual cardiac arrest.
Currently, at Vinmec International General Hospital, fibrinolysis is being applied for emergency treatment of patients with pulmonary embolism. With modern imaging equipment, CT perfusion results are available within 7 minutes and performed routinely.
If you have a need for consultation and examination at Vinmec Hospitals under the national health system, please book an appointment on the website (vinmec.com) for service.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:Daniel R Ouellet, MD, FCCP Associate Professor of Medicine, Wayne State University School of Medicine; Pulmonary embolism, 2020, https://emedicine.medscape.com/article/300901-overview
a4. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Abigail K. Tarbox and Mamta Swaroop, Pulmonary embolism, Int J Crit Illn Inj Sci. 2013, Department of Surgery, Northwestern University Feinberg School of Medicine, Chicago, IL, USA