This is an automatically translated article.
Mesenteric ischemia can affect the small intestine or colon. Accordingly, intestinal ischemia may be secondary to arterial occlusion or may be due to venous outlet obstruction. This is a serious condition that needs to be properly evaluated and intervened actively from the beginning as well as knowing what intestinal ischemia causes in order to promptly prevent it.
1. What is mesenteric ischemia?
Intestinal or mesenteric ischemia (or intestinal ischemia) can affect the small intestine or colon. Of these, acute mesenteric ischemia is the abrupt onset of intestinal hypoperfusion. Patients often present with sudden abdominal pain, which rapidly worsens and requires urgent surgical intervention. In contrast, chronic mesenteric ischemia is seen in patients with mesenteric atherosclerosis, causing intermittent intestinal hypoperfusion that often worsens after meals.
The main causes of mesenteric ischemia include:
Mesenteric artery embolism: The thrombus is usually located in the lumen of the superior mesenteric artery that supplies blood to the small intestine. This condition causes abdominal pain that is often acute in onset. Prognostic factors include cardiomyopathy, atrial fibrillation, recent angiography, vasculitis, and valvular disease. Mesenteric Arterial Thrombosis: Acute arterial thrombosis is usually the result of atherosclerosis either secondary to acute atherosclerotic plaque rupture or gradually accumulates until severe stenosis is present. Predisposing factors include patients with atherosclerosis, peripheral artery disease, hypercoagulable state, estrogen therapy, and prolonged hypotension. Mesenteric vein thrombosis: Mesenteric vein thrombosis increases the resistance of mesenteric venous blood flow. Patients with localized inflammatory processes in the abdomen (such as inflammatory bowel disease) are at higher risk of developing this disease. Patients with hypercoagulability (in other words, patients with inherited and acquired hemophilia as well as malignancies) are also at increased risk. Nonspecific mesenteric ischemia: These are often associated with mesenteric vasospasm, which can eventually cause reduced perfusion to the small and large intestines. Risk factors include peripheral artery disease, septic shock, vasopressors (such as digoxin), cocaine abuse, hemodialysis, and more.
2. What are the manifestations of intestinal ischemia?
To make a diagnosis, the physician needs to take a close look at the personal and family history of patients who may have mesenteric ischemia. Patients with mesenteric ischemia due to acute embolism have a history of prior embolism in approximately 30%. In addition, 50% of people with acute mesenteric vein thrombosis had a personal or family history of deep vein thrombosis or pulmonary embolism.
The most common symptom of intestinal ischemia is abdominal pain. Furthermore, the patient's symptoms and other organ manifestations may help determine the etiology of the ischemic disease. Arterial embolism usually causes sudden, severe pain around the abdomen and is accompanied by nausea and vomiting. Thromboembolic mesenteric artery occlusion is often associated with more severe pain after eating. Patients with mesenteric vein thrombosis often have a slower onset of abdominal pain and a variable intensity.
Sometimes patients with intestinal ischemia have normal physical examination signs. Others may have mild abdominal distention, while peritoneal signs begin to appear when mesenteric infarction and transmural bowel necrosis have occurred.

Thiếu máu ruột gây triệu chứng đau bụng cho người bệnh
3. How to diagnose and treat mesenteric ischemia?
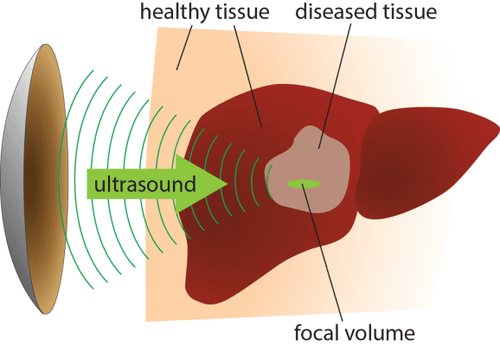
The gold standard for diagnosis of mesenteric ischemia is mesenteric angiography. However, computed tomography angiography is sufficient as the initial diagnostic modality.
Other tests that can help guide the diagnosis are white blood cell count, d-dimer, and lactate, which aid in the diagnosis of mesenteric ischemia, but the clinician should not rely solely on these tests. . In fact, lactate and d-dimer do not have high specificity. A thorough history and physical examination, along with a thorough abdominal exam, are of the utmost importance.
Patients with acute mesenteric ischemia usually require immediate surgical intervention. Treatment should begin immediately in the emergency department with intensive resuscitation with fluid resuscitation and infusion of broad-spectrum antibiotics (covering the gut flora). If the patient remains hypotensive despite intensive fluid resuscitation, norepinephrine infusion should be initiated. In principle, however, vasopressors can exacerbate ischemia and should be used with caution.
Intestinal ischemia due to mesenteric artery occlusion must be treated with early laparotomy with anastomosis. Although still under investigation, some patients with a very early diagnosis of mesenteric artery embolism (without signs of peritonitis) may be treated with local thrombolytic infusion. . Mesenteric artery thrombosis often requires surgical revascularization with mesenteric angioplasty or stenting. In contrast, mesenteric vein thrombosis can sometimes be treated with systemic anticoagulation, but the indication will depend on the severity of the disease.
Finally, as long as there are no contraindications, patients with intestinal ischemia are usually treated with systemic anticoagulation after surgical intervention. In addition, patients should be encouraged to stop smoking and ensure that blood pressure is appropriately controlled. Many patients may develop diarrhea due to ileostomy and may develop short bowel syndrome and malabsorption later, so appropriate post-operative nutrition counseling is required.
4. What is the prognosis and effect of bowel ischemia?
The mortality rate of bowel ischemia is estimated to be between 60% and 80%, especially in those with a diagnosis more than 24 hours late. Surgical intervention within 6 hours of symptom onset increases survival. In general, the prognosis depends on the clinical picture and the etiology of the disease. Patients with arterial etiology have a less favorable prognosis than those with venous etiology.
Regarding complications, mesenteric ischemia can cause many different effects, local or systemic with different degrees. If mesenteric ischemia is not treated in time, complications include:
Necrosis of intestinal tissue Perforation of intestinal wall Peritonitis Generalized septic shock Death

Hình ảnh quai ruột non hoại tử do thiếu máu mạc treo ruột
5. How to prevent bowel ischemia?
The treatment and primary prevention of mesenteric ischemia is an interdisciplinary undertaking. Many of these patients have other comorbidities and need to be evaluated by other health professionals. Because of vascular disease, other body systems also need to be closely monitored.
Specifically, for people with atrial arrhythmias, patients need long-term anticoagulation. In addition, the monitoring physician must also ensure that a therapeutic INR value has been obtained. Routine anticoagulation monitoring is required.
In summary, although the survival of patients with mesenteric ischemia has improved over the past 3 decades, it is still a serious condition with a very high mortality rate. The main treatment methods are still surgery and anticoagulation therapy. However, there is a possibility that intestinal ischemia may recur afterwards; Therefore, patients need to be monitored for a long time, especially with good control of potential risk factors for the disease.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.