This is an automatically translated article.
The article was professionally consulted by Dr. Ngo Viet Thang - Gastroenterologist, Department of General Surgery, Vinmec Ha Long International General Hospital.Rectal prolapse is a common disease common in children 1-3 years old (mucosal prolapse) and people over 50 years old (mucosal prolapse and total prolapse). Although it accounts for only 0.2-1% of surgical diseases and is not too dangerous, it makes many people feel very troublesome because it directly affects daily activities. So what is the cause of rectal prolapse, how to recognize the signs?
1. What is rectal prolapse?
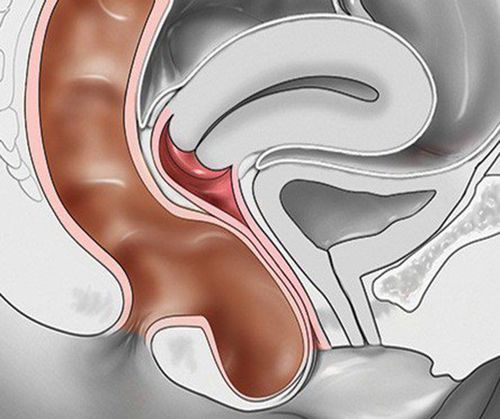
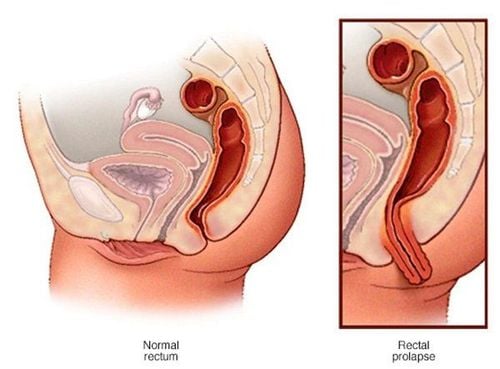
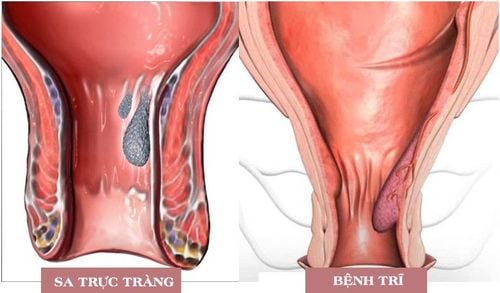
Rectal prolapse is a condition in which part or all of the rectal wall turns over and comes out through the anal opening, a general term that has been used for centuries to describe all types of prolapse. The disease has many different causes and also has many degrees of progression. Therefore, the treatment measures are also very different.Rectal prolapse is divided into 2 main types below.
1.1. Mucosal prolapse
The lining of the anal canal swells and turns upside down every time you have a bowel movement to make it easier to pass stool. After defecation, the mucosal layer shrinks completely because of its elasticity. When the disease occurs, the tissues of the rectum are stretched and stretched often, the mucosa is not only turned beyond normal, but also cannot return. At first, only the mucosa of the anal canal may be prolapsed, and later, the glandular mucosa of the rectum may also be involved.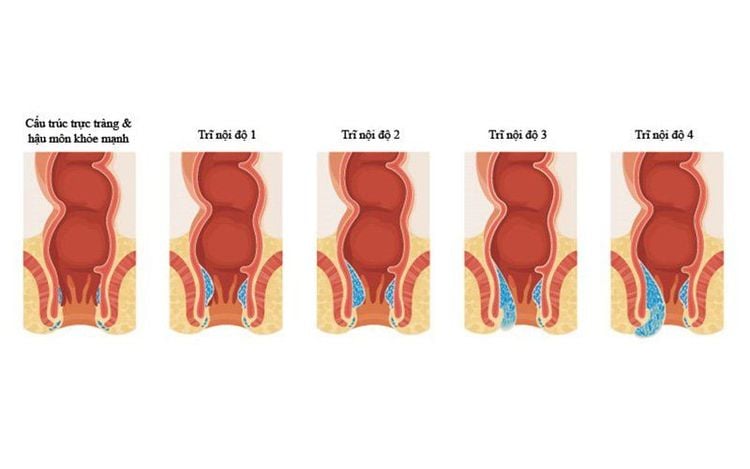
Các mức độ sa niêm mạc.
Mucosal prolapse after straining to defecate and then shrinking by itself. After straining to defecate without self-contraction, it must be pushed up. Falling easily with light exertion such as walking, squatting, coughing, sneezing. Prolapse frequently and continuously outside the anus.
1.2 Sa the whole
Simple rectal prolapse: Only the rectal ball is retracted through the anal canal, the anal canal remains in place. When a finger is inserted into the anal opening, a fold can be seen between the anal canal and the prolapse, and the finger can loop around this division.Prolapse of rectum and anal canal: Both the rectal ball and anal canal are turned out.
Total rectal prolapse is divided into 4 degrees:
Grade 1: The rectum only prolapses when exerting force, when pushing to defecate, then it shrinks quickly on its own. The whole body was not affected, the patient's complaints were only caused by the prolapsed rectal segment. Grade 2: The rectum always prolapses when defecating, it contracts itself very slowly, must be pushed in by the hand, there are slips in the mucosa, edema of the mucosa, the anus is indented, the sphincter changes little, the whole body is normal. often. Grade 3: Rectal prolapse with mild exertion (coughing, laughing, sneezing, walking, squatting,...) and cannot retract on its own. The glandular mucosa of the rectum is necrotic in a few places with scars, the anus loses tone of the flaccid sphincter. Mental repression, mucosal bleeding, bowel incontinence. Grade 4: Frequent prolapse when walking or even when the patient is standing, the bowel can no longer keep in its normal position. The glandular mucosa is ulcerated and necrotic, the wall is scarred, the sphincter is inactive, the bowels are incontinent, and the urine cannot be retained. The patient's mental stress, sensory disturbances in the anal area, the skin around the anus and the groin area; There may be pustules, blisters, itching, eczema in the perineal area. Rectal prolapse is still often considered one of the diseases with puzzling etiology, there are many different surgical treatment methods and the recurrence rate depends on the surgical method used
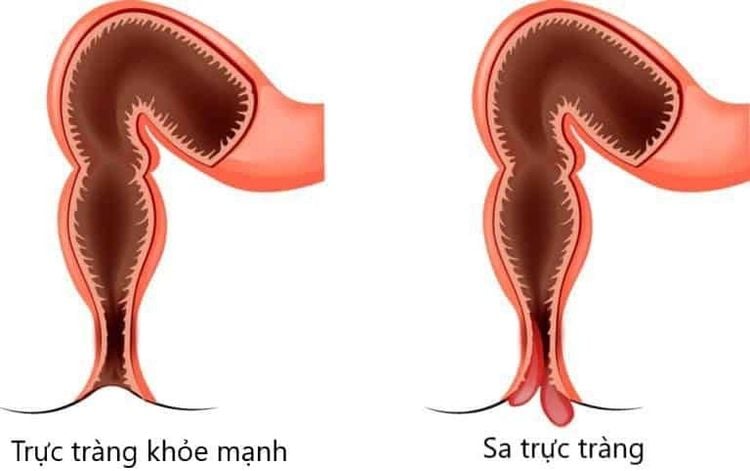
Sa trực tràng với trực tràng bình thường.
2. Causes of rectal prolapse
Causes of sudden and prolonged increase in intra-abdominal pressure.
In children: Diarrhea, whooping cough, narrowing of the foreskin. In adults: Constipation, dysentery, chronic colitis, urinary retention, prostate tumor, bladder stones. Heavy porter. Weakness of the muscles between the anus and rectum
Weakness of the sphincter, the levator of the anus. Weakness of the natural pelvic floor muscles. Anatomical defects
Inadequate means of fixation, especially in the posterior rectum. Loss of physiological curvature of the rectum, loss of anal-rectal angle. The sigmoid colon is too long. The bag with Douglas was too deep and wide. Anal widening. Spasms of the levator and sphincter system.
3. Risk factors that increase rectal prolapse
In children:Previous anal surgery in infancy. Infection. Malnutrition or physical problems. In adults:
Damage due to surgery or childbirth. Weakness of the pelvic floor muscles occurs with age.
4. Signs to recognize rectal prolapse
History of rectal prolapse. The bowel movements are not controlled to a large extent, there may be only mucus discharge. Constipation has also been described as dyspepsia (feeling of incomplete bowel movements) and bowel obstruction. The feeling of being swooped down. Rectal bleeding. Diarrhea and erratic bowel habits. Initially, the prolapsed mass may protrude through the anal canal only during defecation and straining and then return to its original position shortly thereafter. The next time you need to push the prolapse back into place, this can progress to chronic prolapse. Chronic prolapse is defined as spontaneous prolapse that makes walking, standing, coughing, and sneezing difficult because it can cause the prolapsed mass to protrude. The tissue of the rectum with chronic prolapse can undergo pathological changes such as thickening, ulceration, and bleeding. Here are the causes and symptoms of rectal prolapse. Contact your doctor immediately if you have unusual symptoms of rectal prolapse to protect your health.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.