This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
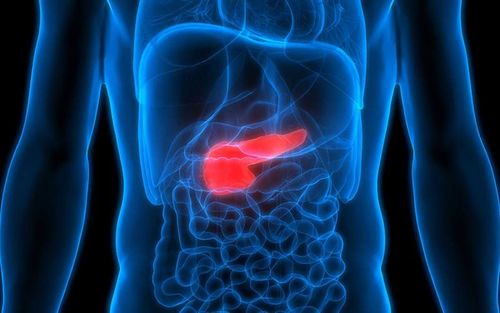
There is a high prevalence of vitamin D deficiency in patients with various disorders of the digestive system, including cystic fibrosis, acute and chronic pancreatitis, celiac disease, short bowel syndrome, and inflammatory bowel disease. In this article, we discuss different causes of vitamin D deficiency and different strategies to normalize vitamin D status in patients.
In general, normalizing vitamin D is beneficial for most patients. However, because there is evidence to suggest that vitamin D can be a negative (reduced) reactant in the acute phase, and thus it is down-regulated in acute pancreatitis, caution may be warranted. when stopping supplementation during the acute phase (and possibly waiting until the acute phase has passed before checking levels) until there is evidence to support benefit.
1. Brief introduction to vitamin D metabolism
Vitamin D has been considered an essential nutrient for the human body until it became clear that it is a natural hormone of the human body. That is, vitamin D is synthesized in the human body and works in ways not unlike a steroid hormone.
However, vitamin D synthesis is special in that it depends on the irradiation of the epidermis of the skin by UV-B (ultraviolet B) rays. In summary, the energy of UV-B photons induces a conformational change in 7-dehydrocholesterol, giving rise to provitamin D3. The provitamin D3 is then naturally isomerized to vitamin D3 (also called cholecalciferol). Vitamin D3 is exported into the blood circulation from the skin and is sequentially metabolized to:
25(OH)D3 (25-hydroxyvitamin D3, or calcidiol) primarily by the enzyme, CYP2R1 (25-hydroxylase), in the liver Then comes 1,25(OH) 2 D3 (1,25-dihydroxyvitamin D3, also known as “calcitriol”) by the enzyme, CYP27B1 (1-α-hydroxylase), in the epithelial cells of the proximal renal tubules. Of the various forms of vitamin D, only 1.25(OH)2 D3 is biologically active. 1.25(OH) 2> D3.
2. Vitamin D deficiency in patients with digestive system disorders
In the blood circulation acts as an endocrine hormone to stimulate vitamin D receptor dependent regulator (VDR) genes for intestinal Ca2+ absorption and renal Ca2+ reabsorption to maintain Ca2+ levels in the blood. healthy blood. 1 PTH (parathyroid hormone) and decreased serum ionized calcium levels induce CYP27B1 activity in the kidney, thereby stimulating the kidney to produce 1.25(OH) 2 D3; Increasing serum levels of 1.25(OH)2 D3, calcium or phosphorus had the opposite effect (decreased CYP27B1 activity). Similar to other hormone systems, 1,25(OH)2D3 has a negative feedback effect on PTH production. Thus, patients with chronic kidney disease have decreased production of 1.25(OH)2D3 and are likely to have PTH hypersecretion and secondary hyperparathyroidism.
Although the proximal renal tubules are the major producer of 1,25(OH)2D3, activated macrophages in extra-adrenal tissues have also been shown to have CYP27B1. Thus, conditions such as sarcoidosis can lead to increased production of 1,25(OH)2D3 in macrophages, which can lead to hypercalcemia. 1,25(OH)2 D3 induced in these tissues acts locally in an intracellular or endocytic fashion to stimulate VDR-dependent gene expression to influence the function of these cells. This explains the potential immunomodulatory effects of VDR-activated synthetic vitamin D analogues shown in several studies. The output of 1,25(OH)2D3 in extra-adrenal tissue is independent of blood Ca2+ and PTH concentrations.
Active ingredient 25(OH)D3 circulates in the blood at a concentration of ng/mL with a half-life of about 15 days while 1.25(OH)2 D3 circulates at a concentration of pg/mL with a half-life of approximately 15 hours. Therefore, blood levels of 25(OH)D3 are often used to determine vitamin D status in the body because of convenience for technical reasons. Although controversial in the literature, vitamin D status is defined by the Endocrine Society as follows:
Vitamin D deficiency is defined as a serum 25(OH) D3 level ≤20 ng/mL Vitamin D deficiency due to serum 25(OH) D3 level 21-29 ng/mL Adequate vitamin D supply according to serum 25(OH) D3 level ≥30 ng/mL. Given the above definition of vitamin D deficiency, vitamin D deficiency occurs in 40-60% of patients with various intestinal disorders, including celiac disease, short bowel syndrome, cystic fibrosis, Crohn's disease and ulcerative colitis. In addition, up to 70% of patients with acute or chronic pancreatitis have vitamin D deficiency. It is noteworthy that more than 40% of patients with acute pancreatitis at the time of admission have severe vitamin D deficiency - that is, serum levels. 25(OH)D3 in their serum was less than 10 ng/ml.

The high prevalence of vitamin D deficiency in patients with intestinal disorders and chronic pancreatitis is strongly correlated with an increased incidence of osteoporosis and low osteoporosis or traumatic fractures.
With the exception of acute pancreatitis, causes of vitamin D deficiency in patients with gastrointestinal disorders seem to include:
Insufficient transdermal vitamin D synthesis Hyperparathyroidism secondary to wasting hypocalcemia calcium Conversion of inflammatory-associated 25(OH)D3 to 1.25(OH)2 D3 However, vitamin D deficiency in patients with acute pancreatitis at the time of admission can be an acute by an as-yet-unidentified mechanism that positively downregulates blood 25(OH)D3 levels during pancreatitis.
3. The rate of synthesis of provitamin D in the epidermis is inversely proportional to the amount of melanin in the skin
Inadequate transdermal vitamin D synthesis in patients due to insufficient solar UV exposure is the main cause of vitamin D deficiency. The rate of pre-vitamin D synthesis in the epidermis is inversely proportional to the amount of vitamin D in the epidermis. melanin content in the skin because melanin is an excellent UV-B absorber, therefore, the prevalence of vitamin D deficiency is higher in darker-skinned patients than in fair-skinned individuals during the same season. Furthermore, because solar UV dose is significantly reduced in geographical locations with high latitudes (>35o North [e.g. Albuquerque, Memphis, Charlotte] or <35o South [Adelaide, Auckland, Melbourne]) in winter due to the zenith angle, the prevalence of vitamin D deficiency in the winter months was much higher than in the summer months for the same patient population. The importance of solar UVB exposure for the maintenance of serum 25(OH)D3 levels is further emphasized by the fact that exposure to sunlight, but not malabsorption, is fat, which is a more important determinant of vitamin D levels in adolescents with cystic fibrosis,7 and the amount of sunlight exposure, but even without oral supplementation up to 800 IU of the vitamin D/day, was the major determinant of serum vitamin D levels over a 4-year period in a cohort of patients with cystic fibrosis.
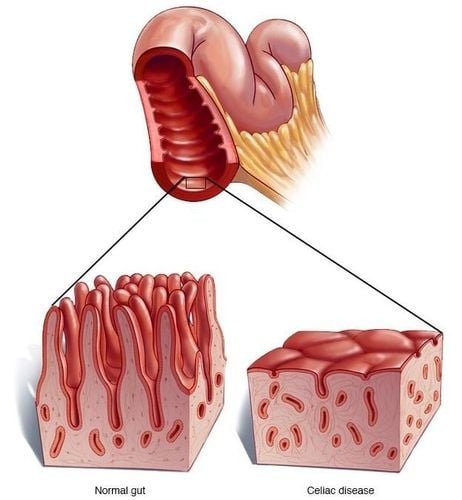
4. Vitamin D deficiency in patients with celiac disease and gastrectomy
Hyperparathyroidism secondary to hypocalcaemia, possibly due to gastrointestinal calcium loss, commonly develops in patients with celiac disease and gastrectomy, and possibly in others with lipodystrophy. Thus, renal overconversion of 25(OH)D3 to 1.25(OH)2D3 by hyperparathyroidism may cause a decrease in serum 25(OH)D3 levels in patients with celiac disease and gastric bypass.
Intestinal conversion of 25(OH)D3 to 1.25(OH)2D during an inflammatory flare is independent of blood levels of PTH and calcium and appears to be primarily cytokine-induced cause inflammation, TNFα, because neutralization of TNF with antibody therapy can effectively restore blood 25(OH)D3 levels in individuals with various inflammatory states. Thus, the conversion of 25(OH)D3 to 1.25(OH)2D3 in the inflamed intestine will "withdraw" 25(OH)D3 from the circulatory system to the inflamed intestine, and thereby reduce 25(OH)D3 OH) D3 in blood levels. The implication of the intestinal production of 1.25(OH)2D during an inflammatory flare-up is that 1.25(OH)2D3 acts locally to activate a biofeedback mechanism to enhance antimicrobial activity. of macrophages and promote intestinal epithelial barrier and tissue healing, and in addition, induce inhibition of proinflammatory T helper cell (i.e. Th1 and Th17) activity in the gut to prevent excessive inflammatory damage in the intestine.
5. Vitamin D deficiency in patients with acute pancreatitis
Severe vitamin D deficiency in patients with acute pancreatitis deserves special attention. In an observational study, 74.4% (58/78) of hospitalized patients with acute pancreatitis were found to be vitamin D deficient (<20ng/mL) during the first 2 days of admission.10 In one study Prospectively, the patient not only reported vitamin D deficiency at the time of admission, there was a gradual decrease in blood 25(OH)D3 levels from day 0 to day 2 as a result of pancreatitis. 25(OH) D3 to 1.25(OH) 2 D3, 2 may lead to hypercalcemia, 16 may cause acute pancreatitis, 1 17 Seems to be active down-regulating 25(OH) D3 levels Beneficial in patients with acute pancreatitis: It will reduce the available substrate for the production of 1,25(OH)2D3 to levels high enough to cause hypercalcemia, which may worsen the condition. acute pancreatitis. Therefore, 25(OH)D3 can be suspected as a negative reactant in the acute phase, especially during acute pancreatitis.
6. Normalization of vitamin D status in patients with disorders of the digestive system
Excluding vitamin D supplements, there are two sources of vitamin D for the human body: Vitamin D found in food and vitamin D3 synthesized in the epidermis when irradiated with UV-B rays. Most natural foods, with the exception of some fatty fish (such as salmon, bluefish, mahi-mahi and swordfish) and a few species of edible mushrooms, are good sources of vitamin D. There are very few foods fortified with vitamin D, such as milk, orange juice, and breakfast cereals. Given the fact that a minimum daily intake of 600 IU of vitamin D is required for those with minimal sunlight exposure to maintain vitamin D, it is impractical for many people to rely on fortified foods. vitamin D to get enough vitamin D3.
7. Sufficient exposure to the sun's ultraviolet rays can lead to the skin's synthesis of the vitamin D the body needs
Therefore, it is important to inform patients that adequate exposure to the sun's ultraviolet rays can lead to the skin's synthesis of the vitamin D required by the body. To determine how much sun exposure to avoid sunburn, doctors can teach patients how to use a solar-powered UV-B calculator developed by Webb and Engelsen. Alternatively, doctors can use short-term UV-B light therapy to stimulate transdermal vitamin D synthesis in patients. 2 However, UV-B light treatments do not appear to be effective for patients with chronic pancreatitis; In addition, patients should be warned that UV-B rays have been added to health risks, such as skin cancer.
8. Vitamin D absorption in patients with ulcerative colitis
Vitamin D absorption occurs mainly in the jejunum and terminal ileum. Therefore, patients with ulcerative colitis, which rarely involves the small intestine, may still have normal intestinal absorption of vitamin D. However, patients with active Crohn's disease or short bowel syndrome have reduced intestinal surface area for vitamin D absorption. Patients with cystic fibrosis and chronic pancreatitis have dyspepsia and fat malabsorption and consequent loss of vitamin D mediated by diarrhea and diarrhea. Decreased intestinal absorption of vitamin D or wasted vitamin D explains why daily intake of up to 800 IU of vitamin D is not effective in normalizing vitamin D status in these patients, and it also explains Explain why normalization of vitamin D status in these patients requires long-term treatment with higher doses of oral vitamin D3 supplements.
9. Supplement with vitamin D3 and vitamin D2
In addition to vitamin D3 supplements, vitamin D2 supplements (ergocalciferol) are also trusted by patients. However, blood levels of 25(OH)D2 (25-hydroxyvitamin D2) cannot be accurately measured by some commonly used methods and therefore the effect of vitamin D2 treatment cannot be accurately determined. on vitamin D levels in the blood. In addition, it has been suggested that the use of vitamin D3 is preferred because vitamin D2 treatment is considered by some researchers to be less effective than vitamin D3 treatment.
Supplemental Vitamin D Doses
Cystic Fibrosis Foundation guidelines recommend that all patients maintain a serum 25(OH)D level of at least 30 ng/ml. Hall et al. reviewed the available evidence and recommended treating cystic fibrosis patients younger than 5 years of age with 12,000 IU of vitamin D3 every two weeks and for older patients with 50,000 IU of vitamin D3 every two weeks.
For most patients with celiac disease, adherence to a gluten-free diet for 6 months or longer can lead to normalization of vitamin D status.
For patients with chronic pancreatitis, long-term vitamin D supplementation with extremely high doses, 20,000 - 60,000 IU/week or even 140,000 IU/week (20,000 IU/day).
For patients with short bowel syndrome, very high doses of vitamin D3 may be needed. In addition, a calcium supplement of 1,500 mg/day should be considered if the patient has impaired bone metabolism.
For patients with Crohn's disease, blood levels of 25(OH)D3 should be raised above 30 ng/ml. Multiple studies have demonstrated that long-term treatment of patients with 2000 IU vitamin D3 per day is necessary to elevate blood 25(OH)D3 levels above 30 ng/ml. In particular, the study by Raftery et al. demonstrated that if the 25(OH)D3 blood level in Crohn's patients in remission is raised above 30 ng/ml, it can reduce the recurrence rate and promote Promotes maintenance of intestinal permeability and increases serum levels of LL-37 (cathelicidin, an antibacterial peptide that promotes intestinal healing and reduces intestinal inflammation) and higher quality of life scores.
However, it should be noted that normalization of vitamin D status in some patients may not be achieved even with super high doses of vitamin D3 supplementation (eg, 10,000 to 50,000 IU of vitamin D3 per day). . Therefore, the vitamin D deficiency symptoms of these patients can be treated with calcitriol (0.5 mg) or bioactive, synthetic vitamin D analogues, such as paricalcitol (1 mg). twice daily, every other day or less often. However, there is no guarantee that calcitriol and vitamin D analogues will be more easily absorbed. In addition, it is prudent for physicians to monitor the blood calcium, phosphate, and PTH levels of their patients to prevent the possible development of hypercalcemia.
CONCLUSION
It appears that increasing blood 25(OH)D3 levels to >30 ng/ml is beneficial for patients with various disorders of the digestive system. To this end, it is reasonable to initiate the patient first on a clinically tried regimen, depending on the disorder, for 2-3 months. If treatment is not achieving the goal, different forms such as tablets (crushed), liquid, or higher doses and longer treatment may be needed; High-dose intramuscular vitamin D3 (“Arachitol”, Solvay Pharmacia) may also be considered. However, patients must be monitored individually on a regular basis to ensure that dose, form, or route of vitamin D adjustments are made in a timely manner.
Finally, although it is currently inconclusive that 25(OH)D3 is indeed an acute phase negative reactant in the setting of acute pancreatitis, due to the production of 1,25(OH)2 D3 is associated with inflammation that can cause Hypercalcemia,16 being the main cause of acute pancreatitis, it is important that clinicians conduct a thorough investigation before deciding to treat patients with acute pancreatitis substitute vitamin D simply because their serum 25(OH)D3 levels were low at the time of admission.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Zhiyong Han, et al., Vitamin D Deficiencies in Patients with Disorders of the Digestive System: Current Knowledge and Practical Considerations. Nutrition issues in gastroenterology, series
153. Christakos S, Hewison M, Gardner DG, et al. Vitamin D: beyond bone. Ann N Y Acad Sci 2013;1287(1):45-58. Adams JS, Hewison M. Extrarenal Expression of the 25-Hydroxyvitamin D-1-Hydroxylase. Arch Biochem Biophys. 2012;523(1):95–102