This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
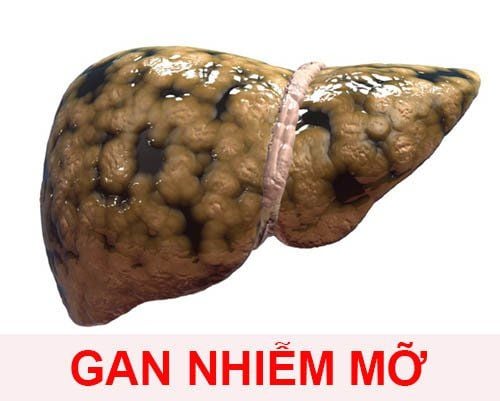
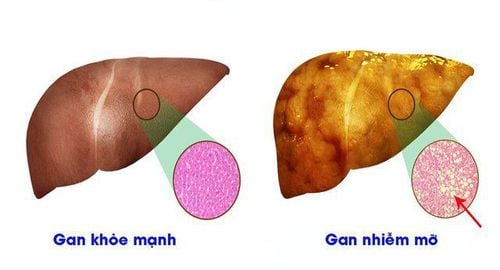
With the growing obesity epidemic and the increasing incidence of metabolic dysfunction-associated fatty liver disease/nonalcoholic steatohepatitis, the management of patients with chronic liver disease becomes quite complex. Patients with metabolic dysfunction-associated fatty liver disease/Non-alcoholic steatohepatitis often have multiple diseases, exhibit different features of the metabolic syndrome, and increase the risk of morbidity and mortality from Heart.
In the early stages of liver disease without evidence of cirrhosis (fatty liver disease associated with metabolic dysfunction), management of comorbidities should guide therapy, while in As patients develop nonalcoholic steatohepatitis and liver fibrosis, liver-related complications and mortality become relevant.
1. The relationship between fatty liver disease associated with metabolic dysfunction and type 2 diabetes
The association between fatty liver disease associated with metabolic dysfunction and type 2 diabetes is well established. Fatty liver disease associated with metabolic dysfunction and type 2 diabetes often coexist, and even in type 2 diabetic patients with normal serum alanine aminotransferase levels, the prevalence of hepatic steatosis is high. . In contrast, many studies have demonstrated a high prevalence of nonalcoholic steatohepatitis in patients with type 2 diabetes, and have also shown that type 2 diabetes is strongly associated with liver fibrosis. Two studies based on liver histology showed that patients with type 2 diabetes often had severe fibrosis, 40.3% and 41.0%, respectively. Other studies, evaluating liver stiffness by transient elastography, showed that 17.7% and 5.6% of diabetic patients had advanced fibrosis. This is of high importance, as liver fibrosis is an important factor in long-term outcomes in patients with metabolic dysfunction-associated fatty liver disease and indeed, fatty liver disease-associated disease. Metabolic dysfunction and type 2 diabetes synergistically lead to increased rates of adverse outcomes including increased liver involvement and overall mortality.
2.The correction of insulin sensitivity is necessary in patients with fatty liver disease associated with metabolic dysfunction
Correction of insulin sensitivity is essential in patients with fatty liver disease associated with metabolic dysfunction, and there is growing evidence that pharmacological treatments are effective in both diabetes type 2 diabetes and fatty liver disease associated with metabolic dysfunction.
Role of Pioglitazone
Pioglitazone, an insulin sensitizer, which stimulates adipocyte differentiation by peroxisome activating receptor g-agonism, has shown beneficial effects on nonalcoholic fatty liver disease. Pioglitazone reduced the severity of non-alcoholic fatty liver disease as assessed by biopsy and liver fat content in patients but also without type 2 diabetes on short-term treatment. Furthermore, a randomized controlled trial showed significantly more frequent resolution of nonalcoholic steatohepatitis in patients treated with pioglitazone (34%) compared with placebo (19%). . However, fibrosis did not improve and insulin resistance was only partially reduced, which may be due to the low dose of pioglitazone used of 30 mg per day. In another randomized controlled trial in nonalcoholic steatohepatitis patients with type 2 diabetes or prediabetes, 45 mg of pioglitazone per day improved tissue nonalcoholic fatty liver disease activity scores. studies, fibrosis and insulin sensitivity. Importantly, the adverse effects of pioglitazone, including weight gain, fluid retention with an increased risk of congestive heart failure, as well as decreased bone mineral density, leading to atypical fractures, should be actively examined. when prescribing pioglitazone in patients with metabolic dysfunction-associated fatty liver disease. Role of glucagon-like peptide-1 (GLP-1) receptor agonists glucagon-like peptide-1 (GLP-1) receptor agonists also represent a valuable therapeutic option for patients Fatty liver disease is associated with metabolic dysfunction, as they improve glucose-dependent insulin secretion, but also promote weight loss and decrease hepatic transaminase levels. In a pilot trial, subcutaneous liraglutide reduced liver fat content and was associated with more frequent resolution of nonalcoholic steatohepatitis, compared with placebo (39% versus 9%). . In contrast, metformin, the first-line type 2 diabetes drug, did not consistently improve steatosis or hepatitis in patients with nonalcoholic steatohepatitis. Overall, however, antidiabetic drugs show great promise in the treatment of metabolic dysfunction/nonalcoholic fatty liver disease (and weight loss) but still require more fully designed randomized controlled trials.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.