This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
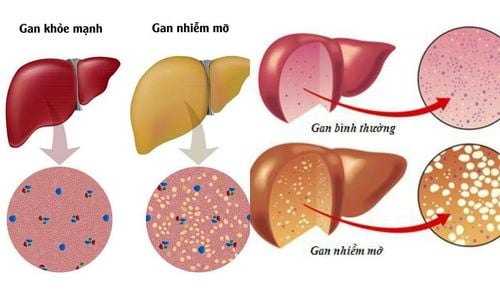
The obesity epidemic has resulted in a significant increase in patients with metabolic dysfunction-associated fatty liver disease (MAFLD). While dyslipidemia, type 2 diabetes, and cardiovascular diseases guide treatment in patients without evidence of liver fibrosis, liver-related morbidity and mortality become associated with the progressive form. of fatty liver disease associated with metabolic dysfunction, non-alcoholic steatohepatitis (NASH), and in the development of cirrhosis. Statins should be prescribed to patients who do not have significant fibrosis despite concomitant liver disease but are used sparingly in a practical setting.
1. Obesity management, diet and exercise
Appropriate treatment for obesity is strongly related, as obesity for each affiliation independently increases the risk for cardiovascular disease and independently predicts clinical compensation in an analysis group of a placebo-controlled trial evaluating beta-blockers for the prevention of esophageal varices, irrespective of the underlying etiology. Furthermore, obese patients, defined as patients with a body mass index (BMI) ≥ 40 kg/m2, had a significantly higher mortality on the waiting list for liver transplantation, and benefited more. from liver transplantation according to Schlansky et al., although cause of death was not reported from the United Network for Organ Sharing registry-based study.
Lifestyle interventions are important
Lifestyle interventions are important, as a 7%-10% loss of baseline body weight has been associated with histological improvement in fatty liver disease associated metabolic dysfunction with reduced steatosis, bullous, and lobular inflammation. An even lower rate of sustained weight loss (about 5%) can reduce obesity, liver enzymes, and the risk of developing type 2 diabetes. Elimination of metabolic dysfunction-associated fatty liver disease by lifestyle interventions has also been demonstrated in non-obese patients with metabolic dysfunction-associated fatty liver disease despite the fact The underlying cause of fatty liver disease related to metabolic dysfunction is unclear. Guidelines suggest that the recommended lifestyle changes structure be made for patients with fatty liver disease associated with metabolic dysfunction and include indicated physical activity including resistance training. resistance, the "Mediterranean" diet restricts calories, avoids high-fructose foods, and avoids excessive alcohol intake. In addition, smoking cessation is important for improving cardiovascular risk profiles.
Diet and exercise are highly effective in treating risk factors
Both diet and exercise are safe in patients with compensated cirrhosis and have been shown to be highly effective in treatment of risk factors (cardiovascular disease and type 2 diabetes, respectively), and reduction of portal pressure in overweight patients with chronic liver disease regardless of etiology. However, it is important that recommendations for weight loss in obese patients with NAFLD/Nonalcoholic steatohepatitis with cirrhosis be extra cautious, because of uncontrolled weight loss in patients with cirrhosis. Decompensation can aggravate weakness and illness. Therefore, it is necessary to plan diligently about diet and exercise to ensure weight loss with adequate amounts of nutrients, especially protein. It should also be considered imperative to investigate whether patients have an indication for non-selective beta-blocker prophylaxis (NSBB) against varicose veins prior to enrollment in an exercise program, because NSBB counteracts exercise-mediated hepatic venous pressure gradient (HVPG) elevation.

2. What do the studies say?
Importantly, evidence from a recently published randomized controlled trial shows that subcutaneous administration of the drug once a week leads to clinically relevant and sustained weight loss (median weight loss). average -14.9% in semaglutide-treated patients compared with -2.4% in placebo, respectively) with a more pronounced improvement in cardiometabolic risk factors and physical activity. Patient-reported in obese individuals without diabetes. Thus, these first encouraging results suggest that more effective pharmacological therapies may be available in the future. Dyslipidemia
Dyslipidemia is a major risk factor for the development and progression of atherosclerotic cardiovascular disease and often presents as a comorbidity in patients with chronic liver disease. Lipid profiles can be altered by liver diseases by impaired cholesterol synthesis, resulting in lipid profiles that appear to improve with progression of chronic liver disease. However, pharmacologically, 3-hydroxy-3-methylglutaryl-coenzyme A reductase inhibition via statins is the most important treatment option for dyslipidemia, resulting in a decrease in systemic levels of high-density lipoprotein cholesterol. low body weight (LDL), as well as systemic effects. In general, statins are well tolerated, however, 10%-15% of patients experience adverse events such as myalgia with or without elevation of creatine kinase.
Is statin therapy safe for patients with decompensated liver disease?
From a liver perspective, long-standing guidelines that statin therapy are contraindicated in patients with chronic liver disease have been shown to be outdated. The authors were able to show that in a real-world setting, statins are underutilized in patients with chronic liver disease. Despite clear indications for the use of statins to reduce cardiovascular morbidity and mortality, outlined in the American Heart Association guidelines, the authors found that 34.2% of patients Chronic liver disease did not progress and 48.2% of patients with advanced chronic liver disease did not take statins despite clear indications, and the authors found that using statins according to guidelines improved rates of Overall survival of patients with compensated chronic liver disease, but no improvement in patients with decompensated chronic liver disease.
Others have found that statins directly affect liver-specific outcomes by reducing the risk of hepatic decompensation, potentially by reducing HVPG, improving hepatocyte function, and ameliorating dysfunction Sinusoidal endothelial dysfunction, overall, indicates that statins should at least be prescribed in non-cirrhotic chronic liver disease patients with cardiovascular risk profiles. In a small pilot trial, simvastatin improved the lipid profile, but not the degree of steatosis and necrotitis, in 16 patients with nonalcoholic steatohepatitis. However, it is also not harmful although the results must be interpreted with caution due to the small sample size.
Overall, most studies have found that, if existing guidelines are followed for initiating statins in patients without decompensated liver disease, the incidence of adverse events is low and the majority of studies Study reports beneficial effects of statins in compensated chronic liver disease, regardless of chronic liver disease etiology
Conclusion
Statins should be prescribed to all patients with compensated dyslipidemia or other factors other risks such as cardiovascular disease but overuse. While there is evidence that statin therapy is safe and also effective in patients with metabolic dysfunction-associated fatty liver disease/nonalcoholic steatohepatitis, large randomized controlled trials still missing. With regard to T2DM therapy, new anti-hyperglycemic agents such as pioglitazone or GLP-1 agonists hold great promise, but specific side effects can be detrimental and must be considered.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.