This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
In recent decades, the proportion of contributions of different causes to the total burden of chronic liver disease has changed. On the one hand, these changes are driven by a 40% reduction in the incidence of hepatitis C virus (HCV)-associated disease in the United States and have resulted in HCV becoming a less common indication for treatment. liver transplantation (LT) in Europe, a trend that is likely to be seen globally in the near future. On the other hand, there is a steady and significant increase in nonalcoholic fatty liver disease, which overall leads to a relative change in chronic liver disease etiologies, and even more absolute increases in the incidence of chronic liver disease. morbidity associated with nonalcoholic fatty liver disease.
While HCV-related liver disease is the domain of hepatologists and transplant units, nonalcoholic fatty liver disease, recently proposed to be re-named as dysfunction-associated fatty liver disease metabolic function, which is associated with extrahepatic diseases, such as central obesity, sleep apnea, type 2 diabetes (type 2 diabetes), cardiovascular diseases, and musculoskeletal disorders, all of which contribute to disease related and affect different specialties
1. The number of liver transplant patients due to cirrhosis associated with nonalcoholic steatohepatitis has increased
Reflecting the obesity epidemic and consistent with changing chronic liver disease etiology, the number of cirrhosis liver transplants associated with nonalcoholic steatohepatitis (nonalcoholic steatohepatitis), the results of The progression of fatty liver disease, associated with metabolic dysfunction, has been markedly increased, with nonalcoholic steatohepatitis having represented the second most frequent cause for liver transplantation in the United States. In addition, the incidence of hepatocellular carcinoma due to nonalcoholic steatohepatitis is also rapidly increasing, which may lead to an even higher need for liver transplantation due to dysfunction-associated fatty liver disease. future metabolic a/nonalcoholic steatohepatitis. Therefore, this review summarizes current treatment options in metabolic dysfunction-associated fatty liver disease, tailored to individual patient stage based on the most recent evidence.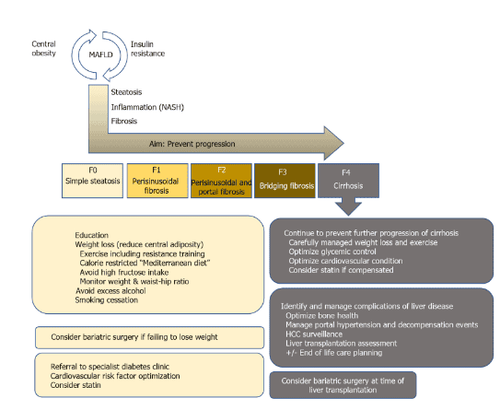
2. Nonalcoholic fatty liver disease/fatty liver disease associated with metabolic dysfunction
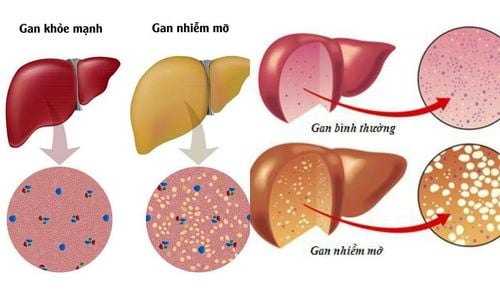
Fatty liver disease associated with metabolic dysfunction is often considered a hepatic manifestation of metabolic syndrome (MS). It was defined as excessive accumulation of liver fat with insulin resistance, steatosis in >5% of hepatocytes in histological analysis (or > 5.6% by fat quantification/selective magnetic resonance imaging). water or proton magnetic resonance spectroscopy), and excluding secondary causes as well as alcoholic fatty liver disease, eg daily alcohol intake <30g for men and <20g for women, usually leads to difficulty Differentiate between alcoholic fatty liver disease and metabolic dysfunction-associated fatty liver disease in retrospective studies.
3. Severity of fatty liver disease associated with metabolic dysfunction
The severity of fatty liver disease associated with metabolic dysfunction can vary from simple steatosis to nonalcoholic steatohepatitis with chronic inflammation and fibrosis to cirrhosis. Unfortunately, up until now, the diagnosis of nonalcoholic steatohepatitis could only be made histologically in the presence of lenticular steatosis, bubbling degeneration of hepatocytes, disseminated inflammation and Mallory-Denk body. This limitation has led to the search for alternative noninvasive diagnostic procedures that avoid the need for liver biopsy.
4. Several factors contribute to the development of fatty liver disease related to metabolic dysfunction
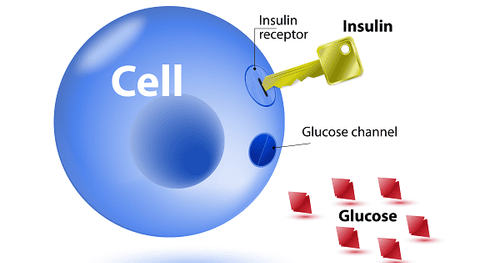
Before fibrosis develops significantly, several factors contribute to the development of fatty liver disease related to metabolic dysfunction, such as diet, insulin resistance, adipokines, gut microbiota, and genetic as well as epigenetic factors. The close link between energy metabolism and fatty liver disease is illustrated by the fact that patients with fatty liver disease associated with metabolic dysfunction have an increased risk of cardiovascular disease, diabetes type 2, as well as chronic kidney disease. According to a meta-analysis by Younossi et al., 51.3% of nonalcoholic fatty liver disease and 81.8% of nonalcoholic steatohepatitis patients were obese, and 22.5% and 43.6% had obesity, respectively. type 2 diabetes, 69.2% and 72.1% had dyslipidemia, respectively. This indicates that diseases should not be treated in isolation because they interact with each other and contribute to disease progression.
5. Patients with fatty liver disease associated with metabolic dysfunction must be considered as multi-metabolic disease
Patients with metabolic dysfunction-associated fatty liver disease should be considered as multi-metabolic disease, as reflected by increased cardiovascular mortality compared with liver-related mortality in people without significant cirrhosis. However, once the liver is fibrosis, liver-related mortality becomes more consistent. Recent evidence from high-quality studies suggests that concomitant fibrosis, and especially cirrhosis, rather than nonalcoholic steatohepatitis per affiliation significantly increases morbidity and mortality. . Thus, well-established tools such as transient elastography with appropriate threshold values can enable risk stratification and identify significant fibrosis, which should offer modern therapy with a liver centered.6. Treatment options in metabolic dysfunction-associated fatty liver disease/nonalcoholic steatohepatitis
As mentioned above, the first step in individual patient risk stratification should be to assess the presence/absence of cirrhosis. In the absence of cirrhosis, regardless of the underlying cause, removal of the damaging agent is important to prevent the development of fibrosis and venous hypertension decompensated events. door afterwards. In metabolic dysfunction-associated fatty liver disease, lifestyle changes should be considered the cornerstone of etiological treatment, as obesity, high-fat diet, and sedentary activity are closely related. development and progression of the disease. Unfortunately, to date, there are no specifically approved pharmacological treatments for metabolic dysfunction-associated fatty liver disease and current trials of fatty liver disease drugs. Associated with metabolic dysfunction or nonalcoholic steatohepatitis are the major metabolic pathways to ameliorate insulin resistance or dyslipidemia.

7. Results of clinical trials
As of 2018, more than 300 substances have been in clinical trials for metabolic dysfunction-associated fatty liver disease/nonalcoholic steatohepatitis. However, the majority of trials have failed to prove effective, and the most effective to date have been alternative drugs such as statins. Regarding newly developed compounds, a recent prospective, placebo-controlled study of obeticholic acid (OCA), a farnesoid X receptor agonist, has been shown to reduce liver fibrosis and reduce inflammation in preclinical studies, showed that OCA improved the degree of fibrosis in patients with nonalcoholic steatohepatitis. Of note, however, complete resolution of nonalcoholic steatohepatitis was no more common in patients treated with intense OCA (placebo: 8%; OCA 10 mg daily: 11%) ; OCA 25 mg daily, 12%), and overall fibrosis improvement was still achieved in only about one-quarter of patients (fibrosis improvement ≥1 stage: Placebo: 12%, OCA 10 mg each day: 18% and OCA 25 mg daily: 23%), highlighting the complexity of treating nonalcoholic steatohepatitis. With this first successful trial, however, it is hoped that a broader range of pharmacological agents will be available in the near future.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.