This is an automatically translated article.
The article was professionally consulted by resident Doctor Le Thanh Tuan - Department of General Surgery - Vinmec Nha Trang International General Hospital. The doctor has extensive experience in examination, treatment and surgery of abdominal diseases.Biliary atresia is a disease characterized by an obstruction in the flow of bile from the liver to the duodenum (small intestine), which can lead to many dangerous complications such as liver abscess, cirrhosis, liver failure or even is death. Treatment of congenital biliary atresia by surgery is an effective method to treat the disease, reducing the risk of complications.
1. Objectives and principles of treatment of biliary atresia in neonates
Goal: Release bile from the liver, eliminate cholestasis, prevent or slow down liver failure; Principle: Surgery as soon as possible. For cases of biliary atresia type I (atrophy of the common bile duct), type II (atrophy of the common hepatic duct), surgery is performed to connect the remaining bile duct outside the liver to the Roux-en-Y jejunum. In case of type III bile duct atrophy (atrophy of the bile duct in the hilar region), Kasai surgery is performed. Patients with bile duct atrophy with end-stage liver failure can undergo a liver transplant.
2. Factors affecting the success of biliary atresia surgery
Age: As an important factor, perform surgery at a younger age, the better the prognosis. The age of surgery with a high success rate is children under 1 month old or within 2 months of age. Children over 2 years old who have just undergone surgery have a relatively high failure rate; Type of biliary atresia: The case of complete atrophy of the extrahepatic biliary tract has a poor prognosis, while atrophy of a part of the extrahepatic biliary tract has a better prognosis; Postoperative cholangitis: Occurs early or late after surgery. Patients need early detection for effective treatment and when operating, doctors should put more anti-reflux valves; The surgeon's experience with the type of surgical technique also affects the success of the surgical method used.
3. Surgical methods to treat biliary atresia
In the treatment of biliary atresia in newborns, the doctor will appoint surgery to unblock the bile ducts, eliminating cholestasis in the liver. The most widely used surgical methods today include:

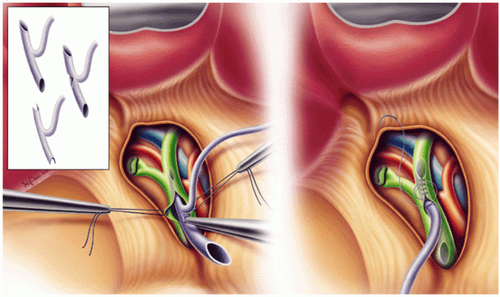
3.1 Common hepaticojejunostomy surgery This method is applied to curable forms of common bile duct atrophy or atrophy of the common hepatic duct. When performing dissection into the hilum of the liver, the doctor will detect a cystic structure, when transversely, there is bile flowing out. This cyst will not be removed but is used to connect to the intestine, creating the flow of bile from the liver to the small intestine.
3.2 Kasai surgery Kasai surgery (enteric-hepatic anastomosis) is named after a Japanese doctor who developed this technique. Kasai surgery can be performed open or laparoscopically. This method is used to treat bile duct atrophy in the hilar region (88% of cases of bile duct atrophy). When performing Kasai surgery, the bile ducts will be removed, a piece of intestine is brought to replace the bile duct connected to the liver hilum, helping to drain the bile produced from the liver. As a result, the outflow of bile from the small bile ducts empties directly into the intestine, bypassing the large bile duct altogether.
3.3 Liver transplant If the Kasai procedure fails, the child needs a liver transplant in the first 1-2 years of life to avoid cirrhosis. In addition, even though Kasai surgery is initially successful, it may not completely restore normal liver function and development. Children with biliary atresia may progress slowly to cirrhosis and related complications, requiring liver transplantation at a later time. Specifically, babies born with fetal biliary atresia need liver transplantation and transplant earlier than those with neonatal biliary atresia. The bile ducts may be more severely affected while the child waits for a liver transplant. Since liver transplantation is indicated for patients with biliary atresia, the 10-year survival rate has risen to over 90%. The main problem is the lack of sources of liver transplants, especially for very young children. Therefore, children are often transplanted with half of the liver of the father or mother. In particular, because healthy liver tissue can grow rapidly, both the baby's and the donor's liver will develop completely over time.
4. Treatment after surgery for biliary atresia
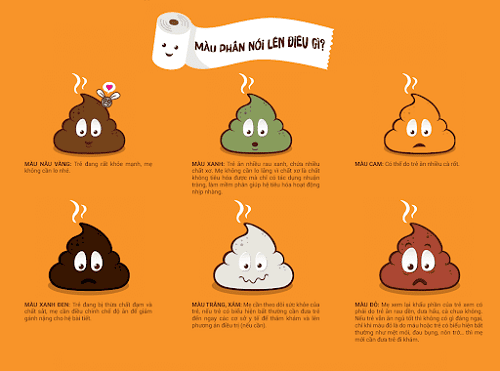
Fasting, providing nutrition through intravenous line until the child passes yellow or green stools after surgery. Depending on the nature and color of stool to adjust the child's daily diet; Eat by mouth after 4 - 7 days when the patient has yellow stools, no fever; Use antibiotics to prevent early biliary tract infections immediately after surgery and in the first 6 months after surgery with prophylactic doses of Cotrimoxazol; Use Ursodeoxycholic (UDCA) at a dose of 15 - 30 mg/kg/24 hours for 18-24 months or until the child stops cholestasis; Supplementing with fat-soluble vitamins such as A, D, E, K for children daily; Supplement calcium and iron in the child's diet;
Use hydrolyzed protein milk with short and medium chain fatty acids; Laboratory tests 1 week and 1 month after surgery (including tests for Protid, Albumin, Bilirubin, GPT, GOT, ALP, CCT),... Re-examination after surgery: In the first 6 months after surgery, re-examination should be once a month; In the next 6 months, re-examination every 3 months and in the 2nd year, periodic examination every 3-6 months.
5. Treatment of complications after biliary atresia surgery
Early complications: Anastomosis, profuse and prolonged abdominal bleeding, electrolyte disturbances, hyponatremia, the patient's family should take the patient to the hospital immediately or notify the doctor for timely treatment; Cholangitis : Found in 40-60%, usually stemming from infection upstream following biliary-intestinal surgery. Manifestations of this complication are fever, decreased bile flow, and increased bilirubin levels in the blood. Pediatric patients with cholangitis need to be treated with intravenous fluids and broad-spectrum antibiotics, susceptible to Gram-negative bacteria. Normally, after 6 - 9 months after surgery, when the flow and bile flow have reached normal levels, cholangitis complications will be minimized; Portal hypertension: At the time of surgery, most pediatric patients have cirrhosis with varying severity - mild. Cirrhosis of the liver causes blood to flow through the liver to slow down, subject to high pressure - also known as portal hypertension. This condition occurs after surgery with a frequency of about 34-76%, affecting the blood flow around the liver. The complication of portal hypertension is gastrointestinal bleeding due to ruptured esophageal varices, seen in 20-60% of pediatric patients after surgery. Pediatric patients should be examined periodically with Doppler ultrasound of the liver and portal vein system, and platelet counts should be assessed. When there are symptoms of portal hypertension, pediatric patients need to have esophagogastroduodenoscopy every 6 months - 1 year to evaluate and prevent gastrointestinal bleeding. Primary prevention of gastrointestinal bleeding due to portal hypertension is with drugs (propranolol), endoscopic interventions (venous ligation, sclerotherapy) depending on the degree of varicose veins. During treatment, it is necessary to pay attention to check the electrocardiogram, echocardiogram, blood sugar, monitor the veins daily and periodically when re-examination. If conservative treatments fail, the pediatric patient may be indicated for portal-host surgery; Malnutrition: It is necessary to consult and adjust the diet to restore nutrition for pediatric patients; Itching: Children with biliary atresia with cirrhosis also often experience itching due to cholestasis in the blood and irritation of nerves in the skin. The doctor can give the child an anti-itch drug, resin or antihistamine, to reduce the sensation of itchy skin; Liver failure: If the liver failure is not reversible, the pediatric patient with biliary atresia after surgery may be indicated for a liver transplant. Surgery is the most effective treatment for children with congenital biliary atresia. For the treatment to be highly effective, with few complications, parents need to strictly follow the doctor's advice in examining and taking care of the child.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.