This is an automatically translated article.
Posted by Doctor Vu Duy Dung - Department of General Internal Medicine - Vinmec Times City International Hospital
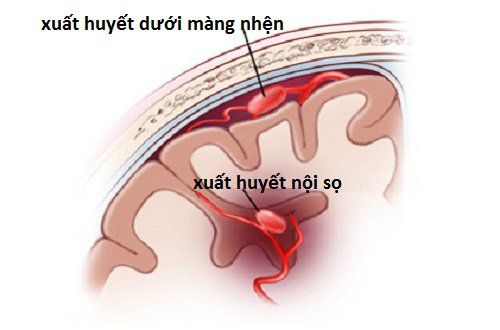
Non-traumatic subarachnoid hemorrhage (SAH) is a type of hemorrhagic stroke that is usually caused by rupture of a sacral (berry-shaped) aneurysm and accounts for about 3% of all strokes.
1. Clinical manifestations of subarachnoid bleeding
Typical SAH presents with a sudden, severe headache (often described as “the worst headache of my life”), which is distinct from the usual headache, and is often accompanied by loss of consciousness, nausea, and vomiting. vomiting, photophobia, and neck pain. A small percentage of patients may have a headache with few or no other accompanying symptoms (guardian headache) and may go undiagnosed or misdiagnosed, thus being missed, with a high risk of major life-threatening rebleeding in a short time (hours to days). Other less typical manifestations, possibly convulsions, acute encephalopathy, and associated subdural hematoma with or without head trauma (because of SAH-related syncope), may make the diagnosis. SAH due to ruptured aneurysm becomes more difficult.
Physical examination should include determining the patient's level of consciousness and Glasgow coma score, evaluation for meningeal signs, and presentation of focal neurological deficits. In cases with uncommon or equivocal presentation, ophthalmoscopy may be helpful. Intraocular bleeding associated with SAH (Terson syndrome) is associated with increased mortality and may be seen in up to 40% of patients with SAH.
Transient elevation of intracranial pressure (ICP) is the cause of nausea, vomiting, and syncope and may be associated with cardiopulmonary complications following SAH. Bleeding in the eyeball in Terson syndrome is thought to be due to a sudden increase in ICP. Severe and prolonged ICP can lead to coma and rapid neurological deterioration leading to brain death.
2. Diagnosis of subarachnoid hemorrhage

Hình ảnh Chụp cắt lớp vi tính
Multiple diagnostic modalities can be used for the diagnosis of SAH
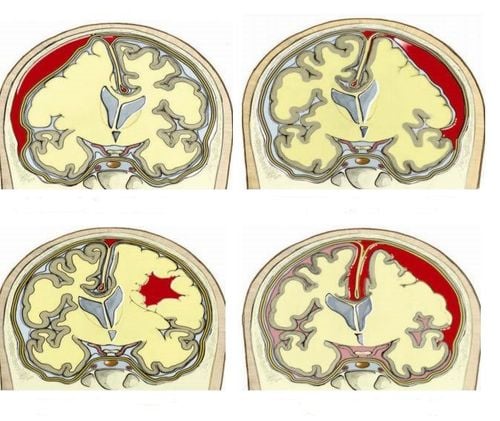
2.1 Computed tomography (CT) of the head
The fastest and most reasonable possible initial diagnostic test for patients with suspected SAH is microscopic tomography The initial calculation did not include contrast injection. It is important to relate head CT results to the time of headache onset, as the sensitivity of head CT varies during the first 7 days from 93% (first 6 h), to close to 100% (first 12 h), to 93% (first day), to less than 60% (first 7 days). Characteristic presentation of hematopoietic hyperattenuation in the basal cisterns or basilar fissures, interhemispheric fissures, and cephalic fissures warrant immediate suspicion of an aneurysm etiology. In fact, any SAH on CT of the head, especially in the absence of a history of head trauma, requires immediate vascular imaging. In addition to the presence of SAH, the physician should also evaluate on the head CT for the presence of hydrocephalus, intraventricular bleeding, and intracerebral bleeding.
2.2 Lumbar puncture
In cases where head CT is negative or equivocal and multiple SAH is still suspected, lumbar puncture is the recommended next step. Opening pressure should be measured routinely. To distinguish puncture bleeding from true SAH, CSF should be collected in 4 consecutive tubes, and red blood cell counts measured in tubes 1 and 4. CSF should be assessed for yellow chromatin by Closely observed with the naked eye and, if possible, spectrophotometrically, for greater diagnostic accuracy than visual observation alone.
Chromosomes take about 12 hours and may not be seen if lumbar puncture is performed earlier after headache onset. Most hospitals do not recommend spectrophotometry, and it is not known what the false-negative rate of chromophore is at different time points after the onset of SAH.
2.3 Magnetic Resonance Imaging (MRI)

Hình ảnh cộng hưởng từ (MRI) trên máy tính
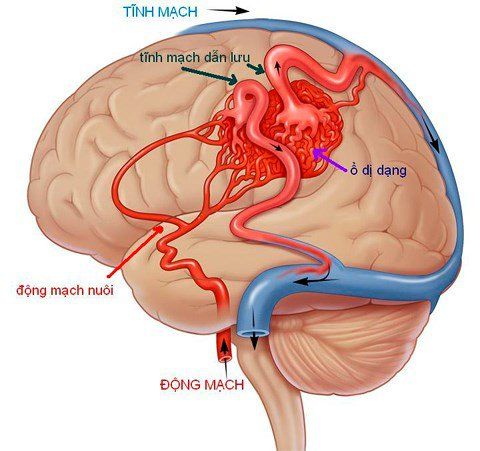
CT and MRI of the head are considered to be equally sensitive in detecting SAH in the first 2 days, except during the first 6 hours after the onset of SAH, when head CT may miss a small proportion of SAH and MRI could be a little more sensitive. Because of the fast imaging results, the wide availability of scanners in the emergency department, and the very high sensitivity in the first 2 days after SAH, first CT remains the diagnostic modality of choice for early SAH. However, sequences of MRI pulses sensitive to hemosiderin (gradient recall echo [GRE] and susceptibility-weighted imaging [SWI]) or FLAIR pulses are more sensitive for detecting subacute or chronic SAH than initial CT. In addition, brain magnetic resonance imaging may be useful in differentiating between pathologic mechanisms, such as arteriovenous malformations and inflammation, infection, and tumor.
2.4 Determine source of bleeding
Vascular imaging should be the next step in all patients with a diagnosis on head CT, lumbar puncture, or MRI. The gold standard of vascular imaging is still digital background deletion angiography (DSA). CT angiography (CTA) is widely used and is now widely used as the primary vascular imaging modality. Depending on technique, slice thickness, and image processing, the sensitivity and specificity of CTA can be 90% to 97% and 93% to 100%, respectively, when compared with DSA. However, CTA may miss small aneurysms ≤ 4 mm.
In the aneurysm and stroke specialist centers, the DSA is available for diagnosis as well as treatment. At the author's hospital, 2D and 3D DSA were followed closely as the golden diagnosis for aneurysms as soon as the diagnosis of SAH was established; CTA was often omitted at the author's hospital to avoid further exposure to radiation, iodine contrast, and its potential for anaphylaxis and nephrotoxicity. Patients with a first negative DSA should have a DSA repeat 7-14 days after the initial scan. In addition, in first-time DSA-negative patients, brain MRI and, depending on SAH location, cervical spine MRI should be performed to look for arteriovenous malformations of the brain, brain stem, or spinal cord.
2.5 Subarachnoid hemorrhage around midbrain
Hình ảnh mô tả dấu hiệu chảy máu dưới nhện quanh não giữa
Approximately 15% of patients with SAH have negative imaging findings for bleeding origin, of these approximately 38% are non-aneurysic midbrain SAH, a particular type of nontraumatic SAH with bleeding confined to the midbrain cisterns. The clinical course has been reported to be more benign, although published case reports demonstrate rare cases of small aneurysms in the posterior circulation, creating a window of vertebral and basilar arteries, or anterior spinal artery abnormalities. So the DSA should still be taken. At the author's hospital, an MRI of the brain and cervical spine, as well as a repeat DSA approximately 7 days after the initial scan, was performed in all cases of periventricular SAH. Patients with periventricular SAH were monitored in a milder unit and, if no source of bleeding could be found, discharged after 8 to 10 days at the author's hospital, provided their hospitalization was not What are the complications?
Source: Susanne Muehlschlegel. Subarachnoid hemorrhage. CONTINUUM (MINNEAP MINN) 2018;24(6, NEUROCRITICAL CARE): 1623–1657