This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Abbreviations
Inflammatory bowel disease (IBD)
Ulcerative colitis (UC)
Crohn's disease (CD)
Intestinal tuberculosis (ITB)
Intestinal Behcet (BD)
Colitis (CAC)
Stained colonoscopy Dye-based Coloring (DBC)
Dye-free endoscopy (DLC).
1. Introduction
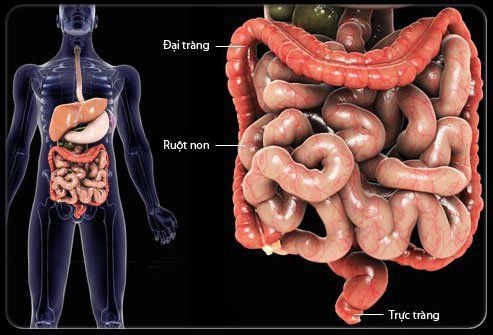
Inflammatory bowel disease (IBD) includes two main types, ulcerative colitis (UC) and Crohn's disease (CD). It is now accepted that both groups of patients have an increased risk of developing cancer-associated colitis (CAC). Chronic inflammation of the gastrointestinal mucosa is an important factor for the development of cancer-associated colitis (CAC). Therefore, chronic use of anti-inflammatory drugs has been suggested to reduce the risk of colitis. However, most studies cannot prove that anti-inflammatory drugs commonly used to treat inflammatory bowel disease have chemopreventive effects against cancer. Therefore, new efforts have been made to better define the development of mucositis in IBD in order to establish more effective targeted and preventive therapies. While all patients with inflammatory bowel disease are at risk of developing colitis, the duration and extent of the disease have been shown to be risk factors for developing cancer. Correspondingly, patients with exacerbations lasting more than 10 years or colitis are at increased risk. Therefore, most guidelines recommend follow-up colonoscopy as the gold standard for the diagnosis of intraepithelial neoplasia and cancer in inflammatory bowel disease.
It is clear that new and more advanced endoscopic imaging techniques are needed to monitor inflammatory bowel disease. In recent years, emerging endoscopic imaging techniques have been introduced, allowing more detailed analysis of mucosa and submucosa. This article describes the concept of advanced endoscopic imaging for the diagnosis and characterization of Crohn's disease.

2. Balloon-assisted small bowel endoscopy
Although standard small bowel endoscopy plays an important role in the management of patients with IBD, its place in the diagnostic and therapeutic algorithm remains poorly defined. The term “balloon-assisted small bowel endoscopy” (BAE) was first proposed by Mönkemüller and colleagues and summarizes three different endoscopic methods for small bowel reconstruction: (1) small bowel endoscopic by double ball (DBE; Fujinon, Tokyo, Japan); (2) single-balloon endoscopy (SBE; Olympus, Tokyo, Japan); (3) NaviAid (Pentax, Tokyo, Japan). All systems allow deep insertion of a colonoscope in the small intestine for diagnostic and therapeutic interventions (eg, for hemostasis, dilation, or biopsy). A combination of oral and anal bronchoscopy is used to examine the entire small intestine.
To date few studies have reported a 30-48% diagnostic yield of DBE when evaluating patients with suspected Crohn's disease. Complications are rare and occur in <1% of cases during balloon angioplasty with a reported risk of perforation up to 3%. However, BAE should not be considered the first-line procedure in the evaluation of suspected small bowel CD, as this procedure is somehow invasive, time-consuming and costly, and is mostly limited to centers specialist center. Therefore, in patients with suspected small bowel CD without GI stenosis, capsule endoscopy should first be considered.
3. Capsule endoscopy
Capsule endoscopy (CE) was introduced in 2002. Currently, many different capsule systems from different companies are available to examine the esophagus, small intestine and colon. The movement of the cyst is passively pushed through the intestine by peristalsis while simultaneously transmitting a color image of the intestine. CE offers the theoretical advantage of visualizing the entire small intestine. However, about 8%-40% of cases cannot reach the cecum. Many studies have shown the impact of CE for the diagnosis of CD-related changes such as ulcers, erosions, erythema, abscesses, and intestinal strictures. In the study of Dubcenco et al. CE yielded a sensitivity and specificity of 89.6% and 100%, and a positive predictive value and negative predictive value of 100% and 76.9%, respectively, for the diagnosis of intestinal CD. not active. However, none of the studies used definitive gold standards, and the diagnosis of Crohn's was always supported by clinical presentation. Therefore, at present the diagnosis of Crohn's disease cannot be based on CE examination alone.
In cases of suspected small bowel, Crohn's disease without intestinal stricture or spasticity, capsule endoscopy should be preferred. Balloon-assisted small bowel endoscopy offers the potential to perform interventions in the small intestine and has a low complication rate.
4. Ambient Laser Endoscopy
Confocal laser endoscopy (CLE) was introduced in 2004 and quickly emerged as a promising method for obtaining real-time in vivo histology during ongoing endoscopy. This technique is based on irradiation of tissue with blue laser light after topical or systemic application of a fluorescent agent. The most commonly used fluorescent agent is fluorescein sodium administered intravenously for systemic tissue staining.
Currently, two FDA and CE certified devices are available. One is integrated into the distal end of the high-resolution endoscope ("integrated", iCLE; Pentax, Tokyo, Japan) and the other represents a stand-alone confocal probe capable of traversing the working channel of most standard endoscopes (“probe-based”, pCLE; Cellvizio, Mauna Kea Technologies, Paris, France).
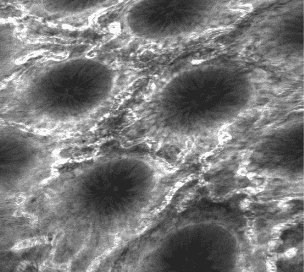
Kiesslich and colleagues impressively demonstrated that a combination of staining endoscopy (methylene blue; 0.1%) and microscopic endoscopy could detect 4.75 times more neoplastic tumors in endoscopic follow-up of UC patients compared with conventional endoscopy. Furthermore, 50% less biopsy samples were required and CLE was able to predict tumor changes with sensitivity, specificity, and accuracy of approximately 95%, 98%, and 98%, respectively. In addition, CLE is also feasible to distinguish between masses or dysplasia-related lesions (DALMs) and sporadic adenomas (adenoma-like masses; ALM) with a high accuracy of 97% and excellent consistency. between CLE and histological diagnosis (κ = 0.91).
A study by Li and colleagues proposed a classification system of inflammatory activity in IBD based on a 4-level classification system of cell pyramidal structure, as well as by analyzing microvascular changes and fluorescence leak. Both, assessment of cytoskeleton structure, and fluorescence leakage with CLE showed good correlation with histological findings. Furthermore, CLE appears to be more accurate than conventional white light endoscopy for macroscopically normal mucosal evaluation. More than half of patients with normal mucosa seen on conventional white light endoscopy presented with acute histological inflammation, whereas none had normal mucosa or chronic inflammation seen on CLE. showed acute inflammation on histology.
Our team evaluated endoscopically for the in vivo diagnosis of histological changes associated with Crohn's disease. Endoscopy can diagnose changes associated with Crohn's disease with great accuracy. Furthermore, microscopy can detect residual inflammatory mucosa that cannot be seen by conventional macroscopic imaging as accurately as histology (kappa value 0.8).
CLE can detect more tumors in surveillance colonoscopy of IBD patients and can predict tumor changes with high accuracy. CLE can reliably predict inflammatory activity in inflammatory bowel disease during ongoing endoscopy, even in patients with endoscopic mucosal abnormalities.
5. Celloscopy
Endoscopy cytology (EndoCyto) allows in vivo microscopic imaging with up to 1390x magnification, thus allowing analysis of mucosal structures at the cellular level. EC is based on the principle of contact light microscopy and thus allows visualization of only the very superficial mucosa. This technique has proven to be reliable for examining mucosal surfaces. In addition, EC can predict neoplasms in foci of malformation and can differentiate tumors from non-tumor colorectal lesions. Our team evaluated the value of endoscopy to identify single inflammatory cells during ongoing endoscopy in patients with inflammatory bowel disease. EC allows clear visualization of various cellular structures in the intestinal mucosa, including cell size, arrangement and density. Furthermore, the size and shape of the nucleus as well as the ratio between the nucleus and cytoplasm were visualized. According to these changes, one can distinguish in real time neutrophils, basophils, eosinophils, and lymphocytes by EC.
EC has the potential to accurately identify various inflammatory mucosal cells during ongoing endoscopy in inflammatory bowel disease and thus the severity of inflammation.
Conclusion
Advanced endoscopic imaging in inflammatory bowel disease has seen a major innovation revolution in the past 10 years, including both live and virtual pigmentary endoscopy. Using capsule endoscopy or balloon-assisted small bowel endoscopy, endoscopists can now assess the entire small intestine and perform endoscopic therapies in a place that has never been visited before. via . Furthermore, recent advances in endoscopic imaging now allow endoscopists to obtain real-time in vivo histology during ongoing endoscopy using microscopy or cytoskeletal endoscopy. .
These emerging imaging modalities allow the endoscope to detect and characterize precancerous and neoplastic lesions and predict mucosal inflammation more accurately than white light endoscopy usually, common, normal. Recent efforts have been made to introduce molecular imaging in inflammatory bowel disease by highlighting inflammatory cells and specific receptors. The results of these trials are highly anticipated and may open new avenues for diagnostic and therapeutic strategies in inflammatory bowel disease.
Vinmec Hospital with modern facilities and equipment and a team of experienced experts, always dedicated to medical examination and treatment, customers can be assured of gastroscopy and esophagogastroduodenoscopy services. at Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference1. Ullman TA, Itzkowitz SH. Intestinal inflammation and cancer. Gastroenterology. 2011;140(6):1807–1816. [PubMed] [Google Scholar]
2. Farraye FA, Odze RD, Eaden J, Itzkowitz SH. AGA technical review on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease. Gastroenterology. 2010;138(2):746–e4. [PubMed] [Google Scholar]
3. Günther C, Martini E, Wittkopf N, et al. Caspase-8 regulates TNF-alpha , epithelial necroptosis and terminal ileitis. Nature . 2011;477(7364):335–339. [PMC free article] [PubMed] [Google Scholar]
4. Neumann H, Vieth M, Langner C, Neurath MF, Mudter J. Cancer risk in IBD: how to diagnose and how to manage DALM and ALM. World Journal of Gastroenterology. 2011;17(27):3184–3191. [PMC free article] [PubMed] [Google Scholar]
5. Rutter MD, Saunders BP, Wilkinson KH, et al. Thirty-year analysis of a colonoscopic surveillance program for neoplasia in ulcerative colitis. Gastroenterology. 2006;130(4):1030–1038. [PubMed] [Google Scholar]
6. Helmut Neumann, Klaus Mönkemüller. Advanced Endoscopic Imaging for Diagnosis of Crohn's Disease, Gastroenterol Res Pract. 2012; 2012: 301541.














