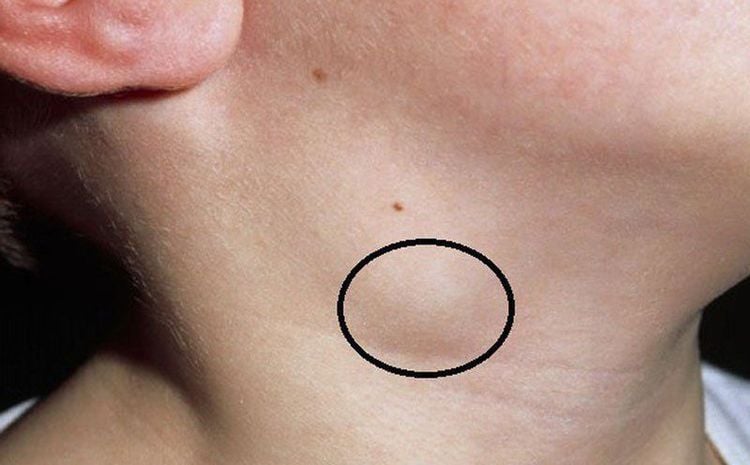
Cervical reactive lymphadenopathy, often referred to as cervical lymphadenopathy, is a common condition characterized by inflamed lymph nodes in the neck. This article will explain the definition and causes of cervical lymphadenopathy, and when you should be concerned about it.
1. What is the definition and causes of cervical lymphadenopathy?
Lymph nodes are small, bean-shaped structures found throughout the body, including the neck, armpits, chest, abdomen, and groin. They are part of the lymphatic system, which plays a vital role in the immune system by helping to fight infections and prevent their spread.
When lymph nodes become reactive, it indicates that they are responding to an issue within the body. Generally, this reaction is not a cause for concern and is considered a normal physiological response. However, if lymph nodes are reacting to an infection or tumor, it may require medical attention.
Many people have experienced enlarged lymph nodes at some point, typically during a cold or infection; this is known as reactive lymphadenopathy.
In children, lymphadenopathy is often associated with infections from microorganisms that enter the body through the mucous membranes or skin of the head or neck to the center lymph nodes.
In particular cases involving pyogenic organisms, such as Staphylococcus or Streptococcus species, the body recruits neutrophils to the lymph nodes. This results in rapid swelling, distension of the capsule, edema, and potential tissue necrosis, along with the risk of abscess formation. Skin erythema and drainage from the lymph node may also occur.
Cervical lymphadenopathy is commonly unilateral, but many acute cases in children are bilateral. The most frequent causes of bilateral lymphadenopathy are colds and streptococcal pharyngitis. The main bacterial culprits for lymphadenopathy are Staphylococcus aureus and Streptococcus pyogenes, which account for 40% to 89% of cases. Other infectious causes include Group B Streptococcus (particularly in infants aged 7–89 days and older patients based on their epidemiology), Yersinia enterocolitica, cat scratch disease, tuberculosis, toxoplasmosis, and lymphogranulomatosis venereum. Less common causes may include tularemia, herpes simplex virus (HSV), Erysipelothrix rhusiopathiae, aspiration anthrax, pulmonary nocardiosis, sporotrichosis, and actinomycosis. This condition can affect both adults and children and can range from acute to subacute or chronic infections.
Certain benign conditions, like osteomas, lipomas, sebaceous cysts, and thyrohyoid cysts, can also lead to cervical lymphadenopathy. These benign tumors or cysts typically do not pose any harm, but proper examination, testing, and diagnosis by specialists are necessary to rule out potential issues.
Tuberculosis can lead to enlarged lymph nodes in the neck. Characteristics of tuberculous lymph nodes include being clustered or stuck together, painless, and having a smooth surface.
Lymphadenopathy can also occur as a side effect of medications such as phenytoin and carbamazepine, or after vaccinations for measles or typhoid. Systemic diseases like HIV/AIDS and lupus erythematosus can also cause lymph node enlargement.
Symptoms of cervical lymphadenopathy include asymmetrical soft lymph nodes, erythema, drainage from the affected nodes, fever, and other signs of systemic infection. Ultrasound can help assess for abscess formation and guide fine needle biopsy. Treatment is based on the underlying cause and may involve oral or intravenous antibiotics, incision and drainage, or surgical removal of the affected lymph nodes.
2. Effective Treatment for Reactive lymphadenopathy
The management of reactive lymphadenopathy varies depending on its cause. Initially, if lymphadenopathies are present in the neck, it is advisable to take the patient to a specialized medical facility for a thorough examination. Healthcare professionals will perform appropriate assessments and order necessary tests to pinpoint the cause of the lymph node enlargement.
Following this diagnosis, treatment will be tailored based on the specific cause and clinical presentation.
In cases where the lymph nodes are swollen, painful, and accompanied by fever, physicians may consider prescribing antibiotics and anti-inflammatory medications, along with analgesics. In more severe situations where pus is present in the lymph nodes, a lymph node puncture may be required for drainage.
It is crucial for patients to adhere to the prescribed medication regimen and to attend follow-up appointments, even if the lymph nodes become non-palpable or symptoms improve. Some forms of reactive lymphadenopathy may resolve spontaneously without antibiotics, requiring only anti-inflammatory treatment and symptom management, along with increased fluid intake.
Patients are encouraged to hydrate adequately and to consume fruit juices rich in vitamin C, such as orange juice and lemonade, to enhance their immune resistance. During the period of lymphadenopathy, vigorous exercise should be avoided.
Typically, benign lymph nodes are more common in children, often resulting from bacterial or viral infections, and tend to be soft or firm, small in size, and develop gradually. In contrast, malignant lymph nodes are more frequently encountered in older adults, though they can also occur in younger individuals. These nodes usually present as firm or hard, less mobile, or deeply situated, and tend to develop more rapidly.
To arrange an appointment, please call HOTLINE or make your reservation directly HERE. You may also download the MyVinmec app to schedule appointments faster and manage your reservations more conveniently.