Coughing up blood (hemoptysis) is the condition of spitting up blood during and after coughing, blood coming out through the mouth or nose due to damage from the larynx down. Diagnosis of coughing up blood due to cancer is usually simple, however, it is necessary to determine the severity of coughing up blood to be able to handle it promptly and quickly, avoiding the risk of death due to acute blood loss and acute respiratory failure due to obstruction or choking on the airway.
1. Common causes
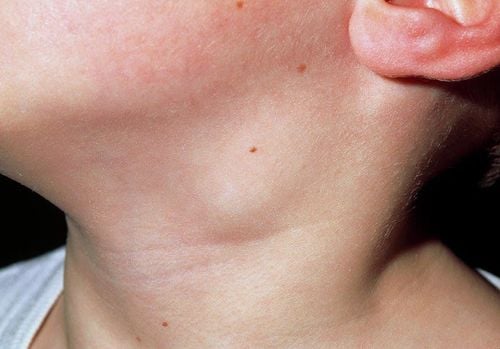
- Coughing up blood is often due to cancers of the head and neck, especially tumors in the hypopharynx and larynx, trachea...
- Lung cancer, especially tumors in the hilum of the lung or tumors invading large blood vessels.
- Esophageal cancer and tumors in the mediastinum can rupture into the trachea.
- Lesions or metastatic cancers, lymphoma, acute leukemia...
Trắc nghiệm: Thử hiểu biết của bạn về bệnh ung thư
Ung thư là nguyên nhân gây tử vong hàng thứ 2 trên thế giới. Thử sức cùng bài trắc nghiệm sau đây sẽ giúp bạn có thêm kiến thức về yếu tố nguy cơ cũng như cách phòng ngừa bệnh ung thư.
Bài dịch từ: webmd.com
2. Clinical symptoms
The patient coughs up blood (hemoptysis) that is initially bright red, foamy and mixed with phlegm, then gradually turns dark.
Clinical examination shows symptoms related to lung and bronchial diseases (fever, shortness of breath, chest pain, rales, crackles, moist rales...).
If the hemoptysis is severe and very severe (like a lightning strike), it can affect the patient's entire hemodynamics, leading to circulatory collapse, the patient has pale skin, pale mucous membranes, low blood pressure, rapid pulse, and acute respiratory failure.
Depending on the severity of the hemoptysis and the lung disease, the patient has rapid breathing, purple lips and extremities.

3. Diagnosis of hemoptysis due to cancer
3.1. Clinical
- Mild hemoptysis: Patients have a condition of coughing up blood or coughing up blood-mixed sputum with a blood volume <50ml/24 hours, hemodynamics are not affected;
- Moderate hemoptysis: Blood volume is about 50ml-200ml/24 hours, pulse may be rapid;
- Severe hemoptysis: Blood volume >200ml/24 hours, if >500ml/24 hours the patient may be in critical condition;
- Thunderclap hemoptysis: Sudden coughing up of large amounts of blood, can cause alveolar apoplexy, suffocation, hemorrhagic shock and death.
3.2. Paraclinical
Blood count test: Red blood cell count, hematocrit, platelets... decrease depending on the level of blood loss.
Blood biochemistry: Perform liver and kidney function tests and electrolytes.
Blood coagulation test: To assess the coagulation status.
Other tests: HIV, HbsAg, blood type...
Acute chest X-ray, CT scan, PET/CT or chest MRI to:
- Evaluate cancer lesions causing hemoptysis: lung cancer, mediastinal tumor, tracheal tumor...
- Exclude other causes: bronchiectasis, pulmonary tuberculosis, pulmonary fungus, Brocq syndrome...
Combine electrocardiogram and echocardiogram to rule out the cause of hemoptysis due to heart valve disease, pulmonary infarction, left heart failure...
Sputum BK test to rule out the cause of hemoptysis due to tuberculosis.
Other exploratory tests:
- Bronchoscopy: Can detect bleeding tumors in the bronchi or localize the location of bleeding lesions, creating conditions for local hemostasis with drugs or a balloon catheter to block the bleeding site, embolization, etc.
- Bronchial angiography: Applied in cases where the patient coughs up a large amount of blood or relapses hemoptysis, the results of angiography can determine the location of the broken bleeding vessel, creating conditions for embolization to stop the bleeding.

4. Treatment of hemoptysis due to cancer
4.1. Principles
- Proceed to promptly and quickly treat symptoms to avoid the risk of acute blood loss, pulmonary aspiration and respiratory failure;
- After the condition is stable, continue to treat the cause.
4.2. Specific treatment
Mild hemoptysis: If there are no signs of respiratory failure, it is necessary to:
- Encourage and explain to the patient and the patient's family;
- Lie in bed, stay quiet, eat liquids and drink cool water;
- Use diazepam 5mg orally or diazepam 10mg intramuscularly;
- Tranexamic acid (Exacyl, transamin): intravenous injection 250mg, 1-2 tubes/time, 1-2 times/day in emergency cases; when the patient is stable, switch to oral form 500mg tablets, 2-4 tablets/day.
Moderate hemoptysis: When the blood volume >150ml
- Glanduitrin intramuscular injection 5 units/tube (should not be injected intravenously because it can cause sudden cerebral vasospasm).
- Glanduitrin 5 units/ampoule diluted in 200ml of 5% glucose solution, intravenous drip, can be repeated 3 times/day (monitor patient's blood pressure, caution should be exercised in patients with hypertension).
- In case glanduitrin is not available or the patient cannot take this drug, morphine 2mg can be used intramuscularly or intravenously every 4 hours or 5mg orally for patients who have not had pain relief with opioids. Increase the dose depending on the case if the patient has taken opioids.
- Combine sandostatin 5 units/ampoule intravenously or mix sandostatin 5 units/ampoule in 200ml of 5% glucose solution or 0.9% NaCl intravenously at 30 drops/minute.
- Infuse high molecular solution (Heasteril 6%) or blood transfusion if the patient has severe blood loss. It is necessary to ensure that the maximum blood pressure is not <110mmHg.
Severe and critical hemoptysis:
- Immediately establish an intravenous line to ensure good resuscitation: Infuse isotonic fluids (0.9% NaCl or ringer lactate).
- Put the patient in the Trendelenburg position on the bleeding side, clean the blood from the nose and mouth.
- Inhale oxygen through a nosepiece or mask at 2-6 liters/minute. If the patient is at risk of choking or respiratory failure, intubation and artificial ventilation should be performed immediately.
- Perform emergency tests: Blood count, biochemistry, chest X-ray, etc.
- Transfuse blood of the same group and high molecular weight replacement products (Heasteril, Gelafundin).
- Vasopressors if the patient has hypotension after adequate circulatory volume compensation (dopamine 200mg x 1 tube mixed in 50ml of 0.9% NaCl infused through an electric syringe starting dose of 5μg/kg/min or noradrenaline 1mg tube mixed with an electric syringe starting dose of 0.1μg/kg/min) gradually increase the dose according to blood pressure.
- Vasopressin, glycerin 1mg, effective for 4-6 hours, intravenous injection 1mg/4 hours, gradually increase the dose to 1.5mg if the weight is over 50kg (note: can cause hypertension, hyponatremia).
- Flexible bronchoscopy to find the bleeding site and perform hemostatic treatment such as: placing a special catheter with a cuff or Fogarty tube, the catheter is inserted into the bleeding area to stop the bleeding, and at the same time washing the bronchi with cold 0.9% NaCl to stop the bleeding.
- Bronchial angiography detects the location of blood vessel rupture in the tumor and performs embolization to stop bleeding. Indications: Coughing up blood >200ml, failing with medical treatment methods.
- In places where conditions are available and the bleeding side has been determined, a double-lumen Carlens catheter can be placed, isolating the bleeding side while simultaneously ventilating the opposite lung and ventilating the healthy lung while aspirating the blood stagnant on the damaged side.
Indications for emergency surgery:
- Hemorrhage in one lung when there are no conditions for bronchial angiography causing obstruction.
- Severe hemoptysis after bronchial artery occlusion.
- Severe hemoptysis affects hemodynamics, causing respiratory failure.
- Surgery is indicated in patients with localized lesions when the general condition and respiratory function allow.
- Surgery is contraindicated in patients with unresectable lung cancer or patients with poor respiratory function that does not allow lung resection.
- Treat the cause when the hemoptysis is stable with the following methods: surgery, radiotherapy, chemotherapy, targeted therapy, immunotherapy...
Currently, early cancer screening is considered the perfect measure for detecting and treating cancers on time. Reducing treatment costs and especially reducing mortality rates in patients. Vinmec International General Hospital always implements and introduces to customers Early cancer screening at Vinmec - Peace of mind to live healthy, helping with genetic testing, imaging diagnosis, and testing of biological markers to detect tumors early. Vinmec International General Hospital has many early cancer screening packages.
- Just one genetic test can assess the risk of 16 common cancers in both men and women (Lung cancer, colorectal cancer, breast cancer, pancreatic cancer, cervical cancer, stomach cancer, prostate cancer, ....)
- Early detection of early signs of cancer through imaging diagnosis, endoscopy and ultrasound.
- The examination is simple, careful and accurate.
A team of experts with professional training, especially in oncology, is capable of handling cancer examinations and treatments.
With advanced and modern medical facilities and equipment and a team of doctors with deep expertise and extensive experience. At Vinmec, the examination process becomes quick with accurate results, saving costs and time for patients.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.