This is an automatically translated article.
Article by Dr. Nguyen Khanh Hoa - Vinmec Stem Cell Research Institute and Gene Technology.Given that inhibition of intestinal peptide degradation leads to DPP4 inhibitors as a novel approach to diabetes therapy, does increasing intestinal peptide secretion also open new therapeutic avenues? Furthermore, can the combination of both methods allow for even stronger glucose reduction and weight loss?
Many other receptors - most of which are G-protein-binding receptors - regulate intestinal peptide secretion in response to nutrients such as fatty acids, amino acids, carbohydrates, and other stimuli. However, despite a large amount of research effort devoted to these receptors, therapeutics have so far remained elusive.
Receptor for bile acids
In addition to aiding in the digestion of fats and soluble fats in food, bile acids activate the nuclear hormone receptor FXR and the G-protein-binding bile acid receptor 1, more commonly known as TGR5. While activation of FXR regulates bile acid synthesis and triglyceride metabolism, activation of TGR5 leads to the production of GLP-1 and PYY from L cells and increased energy utilization, at least in mice. . FXR agonists are currently being investigated for the treatment of NASH with promising results in clinical studies to date. While early studies with TGR5 agonists, such as the bile acid homolog INT-777, have produced potent effects on incretin secretion and glucose release in rodents, adverse effects have been observed. target mediators have so far prevented the inclusion of TGR5 in clinical evaluation. Specifically, TGR5 activation leads to smooth muscle relaxation and stimulation of gallbladder filling, leading to a sharp increase in gallbladder size that cannot be separated from increased GLP-1 or glucose homeostasis. Increased exposition of TGR5 in the gallbladder is the current effort that is focused on reducing systemic exposure of TGR5 agonists by inducing enteric inhibitory compounds.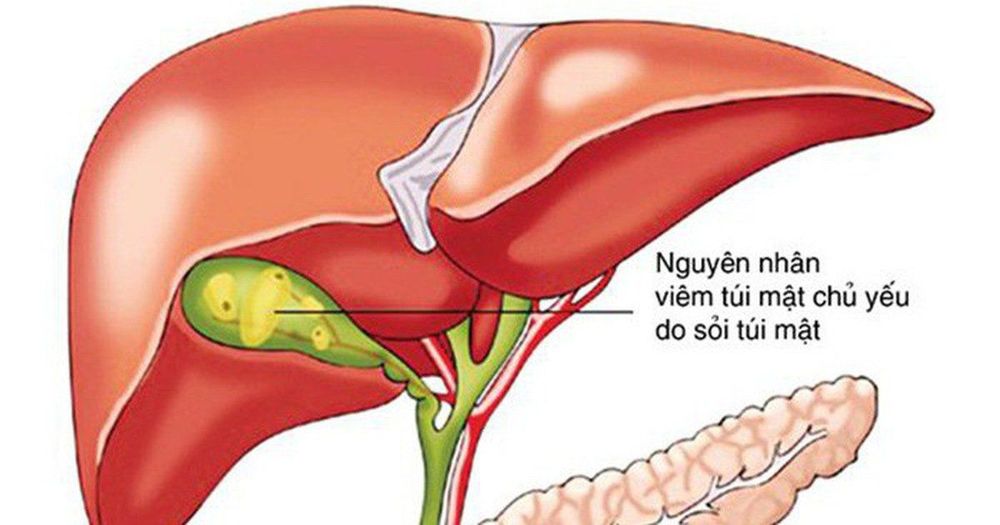
Tăng giải trình của TGR5 trong túi mật là những nỗ lực hiện tại được tập trung
Receptor for long-chain fatty acids and related Lipids
The G-protein-binding receptors GPR40, GPR119 and GPR120 share an affinity for molecularly related and long-chain fatty acids. Interest in GPR119 increased significantly after it was identified as a receptor that mediates the inhibitory effects of 2-monoacylglycerol, specifically oleoylethanolamide, on food intake. In addition, GPR119 was highly expressed in enteroendocrine cells in the intestine as well as in pancreatic islets. Many potent and selective GPR119 agonists have been identified, and preclinical studies show a consistent picture: molecules that induce glucose-dependent insulin secretion and slightly increase GLP-1 and GLP-1 secretion. GIP but had little or no effect on body weight. Clinical studies are done with more than 10 molecules. While a reduction in glucose was observed, the stimulant effect was modest, the impact on GLP-1 and GIP levels was minimal (<50%) and no significant weight loss was observed. These modest effects have resulted in inactivation of the majority of GPR119 agonist studies.The GPR40 agonist was originally developed as a glucose-dependent insulin secretagogue and was later found to also have GLP-1-secreting potential, reflecting the expression of this receptor on pancreatic beta cells as well as on pancreatic beta cells. enteroendocrine cells. A first-generation GPR40 agonist, such as fasiglfam (TAK-875), is a partial agonist that has been shown to lower glucose significantly in the clinic but not to increase both subclinical and clinical GLP-1 levels; No effect on body weight was noted. While discontinuation of fasiglfam is due to concerns about drug-induced liver injury, some partial GPR40 agonists remain in clinical development studies. Recently, full agonists of the GPR40 receptor have been developed that bind to a distinct site and activate both Gaq and Gas signaling. In preclinical studies, these molecules have been among the most potent insulin and incretin secreting drugs described, resulting in 3- to 5-fold increases in blood GLP-1 levels as well as levels of PYY and GIP is elevated, and there is a marked increase in glucose-dependent insulin secretion. However, despite considerable efforts, to date, no full GPR40 agonist has entered clinical trials.
GPR120 is a receptor for long-chain fatty acids expressed in many tissues, most notably adipocytes, immune cells, and enteroendocrine cells of the intestine. Many companies as well as academic investigators have developed small molecular GPR120 agonists and demonstrated glucose-lowering effects in rodents in acute and chronic environments. However, GLP-1 secretion has only been reported in a few molecules with mixed results, and the development of molecules that selectively act on GPR120 remains challenging. To date, no clinical studies with GPR120 agonists have been published.
Receptors for amino acids
A relatively recent nutritional receptor to be discovered is GPR142, now recognized as a receptor for aromatic amino acids that regulates incretin secretion from the gut, as well as glucagon and insulin secretion from pancreatic islets. Selective small molecule GPR142 agonists induce increased insulin and glucagon secretion from rat and human pancreatic islets; improved oral glucose tolerance during acute dosing in lean and obese rats, as well as in monkeys; and improved insulin sensitivity and basal glucose levels upon diet-induced obesity. Circulating intestinal peptides, including GLP-1, GIP and CCK were significantly increased in both rodents and non-human primates with a particularly potent (5-fold) GPR142 agonist having an effect on GIP. Interestingly, the GPR142 agonist was able to induce both beta cell proliferation as well as protect beta cells from stress in isolated pancreatic islets in vitro, suggesting a potential to increase the durability of therapy. . To date, no clinical studies with GPR142 agonists have been reported.Please follow the series on “Effects of the intestine in the treatment of metabolic diseases. Drugs and Future Prospects” by Dr. Nguyen Khanh Hoa:
Part 1: Effect of the gut in the treatment of metabolic diseases. Drugs and Future Prospects Part 2: Intestinal Peptide-Based Approaches Part 3: Other Enteric Peptides-Based Approaches Part 4: Is the gut really the primary source of enteric Peptides? Part 5: Activation of Nutritional Receptors in the Intestine as a Therapeutic Strategy Part 6: Brake Inhibition: Can Somatostatin Antagonists Be Useful for the Treatment of Diabetes?













