This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Researchers are developing a blood test for peanut allergies that could eliminate the need for a sometimes risky and expensive oral food challenge. A new blood test could make diagnosing a peanut allergy a safer and cheaper process.
1. New blood test could provide safer, cheaper way to detect peanut allergy
Scientists from the Medical Research Council in the UK have developed a test that they say poses no risk of false positives or sending patients into anaphylaxis.
Current methods of diagnosing peanut allergy use skin prick or IgE testing to check for specific antibodies. But these tests can lead to overdiagnosis and false positives.
When such tests are not clear, doctors perform an oral food challenge. In this case, the patient was fed peanuts in increasing amounts in a controlled hospital. Although this test is the most reliable way to diagnose food allergies, there is still a risk of serious allergic reactions.
Scientists from the Medical Research Council say their new test is less risky and also 5 times more cost-effective than the oral food challenge.
“Food challenges are the gold standard for diagnosing food allergies... but they carry the risk of allergic reactions, including anaphylaxis. They spent a long time, a day in the hospital. They require equipment and staff with experience in the treatment of allergic reactions and are therefore very expensive, and currently there are long wait times for this procedure in centers that can provide patients ," said Dr Alexandra Santos, a pediatric allergist at King's College London and lead author of the study.
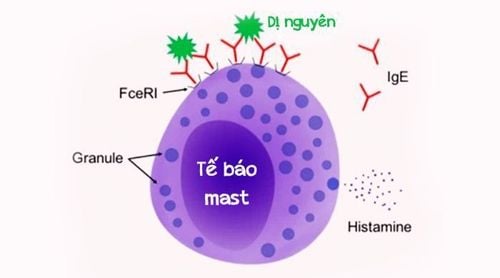
A new blood test, called the mast cell activation test (MAT), can act as an auxiliary tool if the skin prick test results are inconclusive.
“The mast cell activation test can supplement existing tests, such as the skin prick test and the IgE blood test, which are often positive in people without allergies. MAT is highly specific, meaning that when it is positive, it confirms peanut allergy with high certainty, reducing the number of patients requiring challenge and especially the number of patients responding to challenge,” Santos said.
The new test looks at mast cells, which play an important part in triggering allergic reactions.
During the development of the test, researchers used blood samples from 174 children who were tested for allergies. Of these, 73 people are allergic to peanuts and 101 people are not allergic.
Researchers added peanut protein to mast cells and then screened for activated mast cells.
They said the MAT identified peanut allergy with a specificity of 98%. The test also showed the severity of the peanut allergy. The more mast cells are activated, the more severe the response.
2. A promising alternative
Allergy experts say the new test sounds promising. “This could be a game changer if the data supports the accuracy of the test and the reliability of the proper diagnosis,” said Tonya Winders, executive director of the Allergy and Asthma Networks of America America, has said.
“At this time, the oral food challenge is the only definitive test to determine if a person really has an allergy. This new test holds promise for a less invasive, less risky option to make this diagnosis,” she added.
Santos says current allergy tests are not ideal and can produce misleading results. “Only 22% of school-age children in the UK who tested positive for peanuts were actually allergic when they were fed the food in a supervised environment,” she said.
Dr Richard Lockey, director of the division of Allergy and Immunology at the University of South Florida School of Medicine, says overdiagnosis of food allergies is a common problem.
He said: “The usual doctors know very little about allergies, especially food allergies, so when they see a positive result, they tell the patient not to eat that food, even though they ate that food with no problem. “A food test should not be performed unless there is a history of a positive reaction to a food, in this case peanuts.”

3. What are the future goals?
It may still be a few years before this test is used regularly. The researchers are also adapting the test for other uses. “We are currently developing this test for other food allergies, such as milk, eggs, other nuts and seeds. In addition to diagnostic applications, MATs can be used to monitor improvement in patients being treated for food allergies and detect the presence of food allergens in food,” - Santos said.
If the test is made available for widespread use, the number of people who need to take the oral food challenge will be reduced, as will the risk of associated allergic reactions.
Santos says this will make allergy testing for patients much more pleasant, as well as more accurate.
“The new test is specific in confirming the diagnosis so when it's positive we can be sure it means an allergy. We will reduce the number of stressful and costly oral food challenges by two-thirds, and save children from allergic reactions,” said Santos.
The above information is for reference only, you should consult your doctor before deciding to use any treatment method.
At Vinmec International General Hospital, there is a package of examination and advice on treatment of atopic dermatitis to help customers assess the overall condition of the disease and advise on measures to help prevent recurrence.
When registering for a package of examination and consultation for treatment of atopic dermatitis, customers will receive: Dermatology specialist examination. Perform tests such as: quantitative IgE, fresh mycobacteria, specific IgE quantification with respiratory allergens - food (Panel 1 Viet), test Rida Allergy Screen (panel 1)...
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Healthline. New Blood Test May Provide Safer, Cheaper Way to Detect Peanut Allergies