This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalEosinophilic gastroenteritis (EGE), a type of eosinophilic gastrointestinal disorder (EGID), is a rare chronic inflammatory disease characterized by patchy or diffuse infiltration of the gastrointestinal tract. eosinophils into different layers of the gastrointestinal tract. Exact epidemiological data are lacking as most current studies are limited to small case series and single case reports.
1. Is eosinophilic gastroenteritis common?
The incidence of eosinophilic gastroenteritis is estimated to be around 1-30/100000. Furthermore, no effective consensus statement exists to guide clinical practice and remains a challenge. for clinicians in the diagnosis of eosinophilic gastroenteritis. Although recent studies and case reports have demonstrated an increasing incidence of eosinophilic gastroenteritis, we believe that the prevalence of eosinophilic gastroenteritis is increasing. is underrated.Eosinophilic gastrointestinal disorder (EGID) was first described by Kaijer in 1937 and is characterized by eosinophilic infiltration of various layers of the gastrointestinal tract with no known cause secondary. Eosinophilic dyspepsia is mainly associated with eosinophilic esophagitis (EoE) and eosinophilic gastroenteritis (EGE). In Asian patients, EGE occurred more frequently EoE than in Caucasian patients.
How many patients with eosinophilic gastroenteritis worldwide are missed and how does this happen? Very few studies have sought to answer this question. To improve clinicians' understanding of eosinophilic gastroenteritis and to increase diagnosis rates, clinical features of patients with eosinophilic gastroenteritis were treated. at the hospital has been retrospectively summarized by many authors. For patients who had undergone gastroscopy and colonoscopy and whose pathology showed only chronic inflammation in the medical record, study groups were enrolled; noted the probability that a diagnosis of eosinophilic gastroenteritis was missed and subsequently re-examined. Finally, patients with upper gastrointestinal tract discomfort for at least one month were included in the study, and the probability of a missed diagnosis of eosinophilic gastroenteritis was investigated preoperatively. rescue.

2. Why is the diagnosis of eosinophilic gastroenteritis missed?
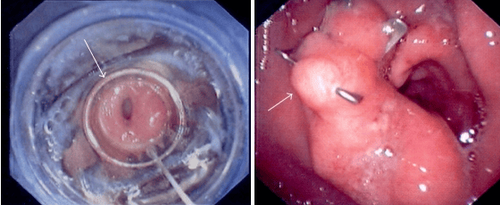
According to previous studies, the incidence of EGE has been estimated at 1-30/100000. Recent studies and case reports have demonstrated that the incidence is increasing. In their study, Reed et al revealed that of all the biopsies obtained endoscopically at their center, 0.67% of them met the criteria for EGE. This suggests that EGE is not as rare as previously thought. Rates of missed EGE diagnoses can be very high. A multi-author retrospective study showed a 4.26% chance of a missed diagnosis of EGE in patients with gastroscopy and histopathology showing only chronic inflammation. Their study also showed a 4.40% chance of a missed diagnosis of EGE in patients whose colonoscopy and histopathology showed only chronic inflammation. A prospective study found that 5.74% of patients had chronic upper gastrointestinal complaints that could represent missed diagnoses of EGE. Thus, the incidence of eosinophilic gastroenteritis is being underestimated, not only because the incidence of eosinophilic gastroenteritis is increasing but also because the diagnosis is easy to miss. eosinophilic gastroenteritis in clinical practice.Because of the nonspecific nature of the symptoms of eosinophilic gastroenteritis, especially in patients with mild symptoms, many clinicians rarely think of eosinophilic gastroenteritis. eosinophils unless these symptoms are bothersome or eosinophilia in the peripheral blood. It is well known that not all eosinophilic gastroenteritis patients have elevated peripheral blood eosinophils, which may lead to missed diagnoses in some patients with high blood counts. Normal peripheral blood eosinophils. Furthermore, the definitive diagnosis of eosinophilic gastroenteritis is often based on gastrointestinal endoscopy and histopathology, specifically to determine the total number of eosinophils infiltrating over a high power field, but the Pathologists do not accurately assess eosinophil infiltrates unless the clinician has a special request to do so.
Regarding the reasons for the missed diagnosis of eosinophilic gastroenteritis, we review the nonspecificity of the symptoms and endoscopic presentation of eosinophilic gastroenteritis, the understanding Inadequate knowledge of eosinophilic gastroenteritis and lack of communication between clinician and pathologist, among other reasons. The clinical manifestations of eosinophilic gastroenteritis are highly dependent on the location and depth of eosinophil infiltration. The most common clinical manifestations were abdominal pain, nausea, vomiting, diarrhea, weight loss, abdominal distension, dysphagia and, in some cases, gastrointestinal bleeding. Most patients with eosinophilic gastroenteritis do not present with any specific symptoms, and this number can be as high as 80% of all eosinophilic gastroenteritis patients. As in the study of many authors, these patients always present with abdominal pain, epigastric discomfort, abdominal distension, nausea and vomiting, diarrhea and other symptoms.

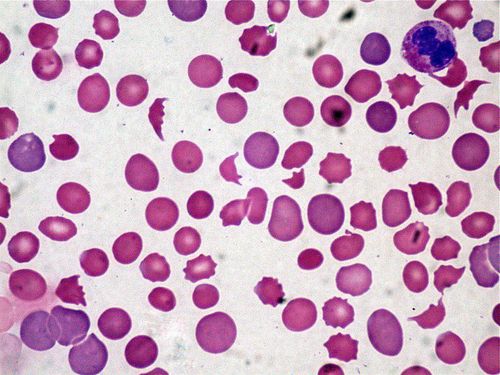
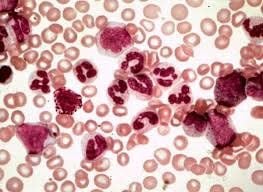
An increase in the level of peripheral eosinophils is an important factor in the diagnosis of eosinophilic gastroenteritis. It is well known that not all eosinophilic gastroenteritis patients have elevated peripheral blood eosinophils. Current studies show that approximately 70%-90% of patients with eosinophilic gastroenteritis have elevated peripheral eosinophil counts. According to a retrospective study by several authors, almost all patients with eosinophilic gastroenteritis had elevated peripheral eosinophil counts, whereas in a prospective study of some authors In contrast, only about 30% of patients diagnosed with eosinophilic gastroenteritis have elevated peripheral eosinophil counts. Therefore, a high level of peripheral eosinophils is important in the diagnosis of eosinophilic gastroenteritis, but it is not mandatory. Waiting to observe an increase in peripheral eosinophils before considering eosinophilic gastroenteritis is a major mistake, often leading to missed diagnoses and medical tests. unnecessary. Therefore, we believe that a missed diagnosis of eosinophilic gastroenteritis occurs more readily in patients with mild presentation and who have a better overall condition.
Since normal levels of peripheral eosinophils are seen in some patients with eosinophilic gastroenteritis, evidence of one or more areas of the GI tract infiltrated by eosinophils is more reliable and necessary for diagnosis. Unlike the esophagus, a healthy digestive tract usually contains a certain number of eosinophils. Therefore, different studies have identified infiltrative eosinophil counts as a marker of pathological infiltrates to varying degrees. The stomach and small intestine, especially the antrum and duodenum, are the most affected sites in eosinophilic gastroenteritis. According to studies, an antrum biopsy should be performed, and at least 5-6 biopsies should be obtained to improve the positive detection of eosinophilic infiltrates. One study confirmed that nearly 50% of patients with eosinophilic gastroenteritis had abnormal eosinophils in the colon and rectum. Therefore, for patients with suspected negative results by gastroscopy, colonoscopy is necessary to collect evidence of eosinophilic gastroenteritis. Furthermore, in some cases, repeat endoscopy may be helpful. More importantly, because pathologists do not routinely calculate eosinophil counts on biopsies, a special reminder should be sent to pathologists when gastroenteritis is suspected. eosinophils.

Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesKodjo-Kunale Abassa, Xian-Yi Lin, Jie-Ying Xuan, Hao-Xiong Zhou, Yun-Wei Guo. Diagnosis of eosinophilic gastroenteritis is easily missed. World J Gastroenterol. May 21, 2017; 23(19): 3556-3564 Hirano I, Moy N et al (2013). Endoscopic assessment of the esophagus features of eosinophilic oesophagitis: validation of a novel classification and grading system Gut, 62(4),: 489 -95