This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalEosinophils are one of the components of white blood cells produced in the bone marrow and are one of the cells that play a role in promoting inflammation, especially allergic inflammatory reactions. Therefore, large quantities of eosin can accumulate in tissues such as the esophagus, stomach, small intestine and sometimes in the blood when such individuals are exposed to the allergen.
1. Eosinophilic gastroenteritis
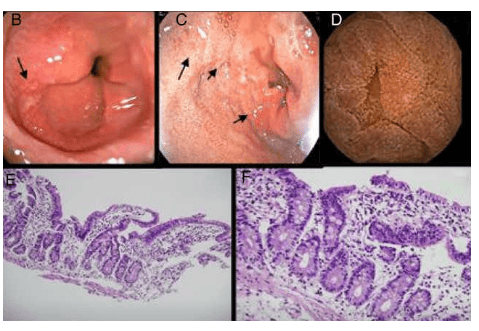
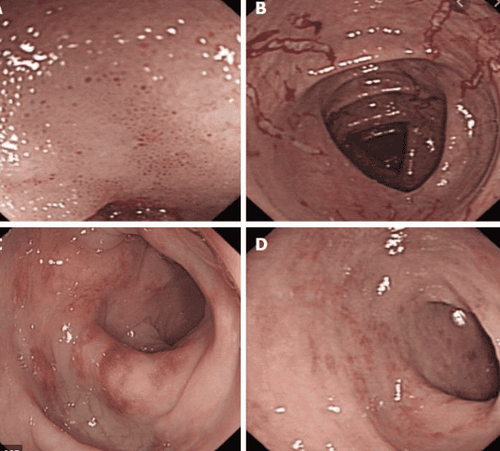
Eosinophilic gastroenteritis (English used from Eosinophilic gastroenteritis_EG) is a disease in the following group of diseases: eosinophilic esophagitis (eosinophilic esophagitis), gastritis, enteritis, colitis eosinophil gastritis, enteritis, and colitis), and members of this family of diseases are collectively known as eosinophilic gastrointestinal disorders (EGIDs). Although rare, eosinophilic gastroenteritis should be recognized by the clinician as soon as possible because the disease presents with signs, symptoms, and syndromes that are "similar" to some other diseases. other digestive disorders, especially peptic ulcers, but with proper treatment, the disease still cannot be cured. Furthermore, eosinophilic gastroenteritis is treatable, sometimes presenting as masquerade as the irritable bowel syndrome. The diagnosis of EG is confirmed by biopsy or collection of eosinophilic ascites in the absence of other pathogens, including intestinal parasites. Eosinophilic esophagitis should also be differentially diagnosed and discussed. Another point to note is that the disease often manifests in one or more family members of the patient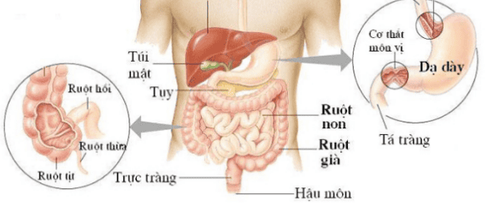
2. Treatment of eosinophilic gastroenteritis
To date, there is no recommendation or consensus regarding the management and treatment of eosinophilic gastroenteritis due to the lack of large sample size, randomized controlled clinical trials. Currently used therapies include nutritional therapy, corticosteroids, and some other drugs. In case the patient has complications of perforation or intestinal obstruction, surgical indications should be made.2.1 Diet Eosinophilic gastroenteritis patients have a high incidence of food allergies so the use of an allergen-eliminating diet or a formula diet is recommended. Adoption of this diet reduces the dose of corticosteroids required as well as improves growth rate in sick children. However, in clinical practice, the use of an elimination diet based on the results of allergy tests produces mixed results because the patient response is not related to food sensitization. The diet traditionally excludes allergenic foods, especially soy milk, eggs, wheat, nuts, and fish, and then reintroduces each to determine if the allergen has been identified. applied in patients with eosinophilic gastroenteritis. Results showed symptom improvement in both adults and children. In addition, a formula diet consisting of only essential amino acids can be effective, but high cost and reduced quality of life are barriers to its application.

Predisone or budesonide may be used. The dose of prednisone is 0.5 - 1 mg/kg until clinical remission is achieved in about 2-14 days. Then gradually reduce the dose over 6 to 8 weeks until prednisone is completely stopped. Budesonide may be an alternative in maintenance therapy with the advantage of low systemic effects. The dose to achieve complete remission with budesonide is 9mg/day followed by a maintenance dose of 3-6mg/day.
2.3 Other drugs Mast cell inhibitors : Disodium cromoglycat is a mast cell stabilizer that prevents the release of toxic mediators from mast cells such as histamine, platelet activating factor, leukotriene. Several studies have documented that the use of disodium cromoglycate may produce a clinically relevant response. Ketotifen, an antihistamine and mast cell membrane stabilizer, has also begun to have case reports of clinical improvement with doses of 2-4 mg/day. Azathioprine: Dosage will be the same as for IBD patients (2 -2.5 mg/kg). The efficacy of azathioprine in patients with steroid-dependent and refractory eosinophilic gastroenteritis has been demonstrated. Leukotriene receptor antagonists: Montelukast is a selective eukotriene receptor antagonist that is relatively safe and holds promise as maintenance therapy especially for patients with steroid dependence. Several studies have reported that the use of Montelukast at doses of 10-40 mg/day for several months is effective in both clinical symptoms and in reducing peripheral blood eosinophil counts.
Anti-IL5 antibody: Several studies with small numbers of patients have demonstrated the efficacy of this monoclonal antibody in patients with eosinophilic syndrome and in patients with leukemic gastroenteritis. craving.
Antihistamines : Currently not the first choice in the treatment of eosinophilic gastroenteritis due to data coming mainly from experimental studies.
2.4 Surgery Cases of eosinophilic gastroenteritis The muscle may present with intestinal obstruction due to the thickening, edema of the intestinal wall, narrowing of the gastrointestinal tract. These cases may respond to corticosteroid treatment. Cases of intestinal obstruction requiring surgery should be guided on nutrition and medical treatment to avoid recurrence.
Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic and treatment techniques for digestive diseases. Along with that, at Vinmec Hospital, the diagnosis of gastrointestinal diseases is done through gastroscopy and colonoscopy with Olympus CV 190 endoscope, with NBI (Narrow Banding Imaging - endoscopy) function. endoscopic examination with narrow light spectrum) results in clearer mucosal pathological analysis results than conventional endoscopy, detecting inflammatory lesions, early gastrointestinal cancer lesions. Vinmec Hospital with modern facilities and equipment and a team of experienced experts who are always dedicated in medical examination and treatment, customers can rest assured with the gastrointestinal endoscopy service at the hospital. Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:Dao Van Long, Dao Viet Hang. Autoimmune diseases of the gastrointestinal tract. Medical Publishing House. Oyaizu N., Uemura Y., Izumi H, et al (1985). Eosinophilic gastroenteritis. Immunohistochemical evidence for IgE mast cell-mediated allergy. Acta Pathol Jpn, 35(3), 759-766. 3. Talley N, J., Shorter R. G., Phillips S. F. et al (1990). Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues. Gut, 31(1),54-58. Brito-Babapulle F. (2003). The eosinophilias, including the idiopathic hypereosinophilic syndrome. Br J Haematol, 121(2), 203-223. 11 5. Pineton de Chambrun G., Desreumaux P., and Cortot A. (2015). Eosinophilic enteritis. Dig Dis, 33(2), 183-189.