This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International Hospital
White blood cells circulate in the blood circulation and help the immune system fight infections. When an infection or inflammation occurs, the body releases white blood cells to help fight the infection.
1. What are eosinophils?
Eosinophils are one of the three components of granulocytes, which are produced in the bone marrow and are one of the cells that play a role in promoting inflammation, especially allergic inflammatory reactions. Therefore, large quantities of eosin can accumulate in tissues such as the esophagus, stomach, small intestine and sometimes in the blood when such individuals are exposed to the allergen. The allergens that cause this EE esophagitis are not known, only that they enter through inhalation or ingestion.
Under normal conditions, eosinophils (BCAT) can be found in different parts of the gastrointestinal tract, except the esophagus. These cells play an important role in the innate immunity mechanism with the function of protecting against various invaders. Eosinophilia in the gastrointestinal tract can be seen in many diseases such as infections, parasites, chronic inflammatory bowel diseases, eosinophilic syndromes, connective tissue diseases, proliferation Malignant marrow, hypersensitivity to drugs. If it is not due to the above causes, it is necessary to consider whether it is eosinophilic gastroenteritis. Eosinophilic esophagitis has been covered in a separate article (Eosinophils and Eosinophilic Gastroenteritis) so this article is mainly about eosinophilic gastroenteritis. acidosis (VDDRDBCAT). This is a major histopathologically based short leg disease with elevated BCAT counts in gastrointestinal mucosal biopsies and local causes of BCAT elevation. However, the criteria for histopathology to date have not been agreed, so the role of the pathologist in conjunction with the clinician is very important.
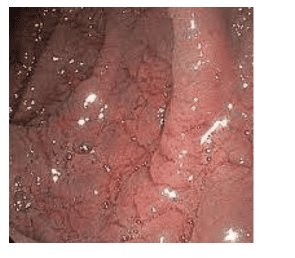
To date, there is no consensus or specific guidance on the diagnostic approach in VDDRDBCAT. Therefore, in clinically suspicious cases, multiple biopsies (4-5 pieces/site) should be obtained from the gastric mucosa or colon for confirmation. In addition, taking a careful history, combining laboratory results, imaging studies and endoscopy helps to rule out other possible causes of increased BCAT in the gastrointestinal tract.
2.Causes of eosinophilia in the gastrointestinal tract
Secondary causes of gastrointestinal elevation of BCAT include:
2.1 Elevated BCAT syndrome (HES) This syndrome is defined as an elevation of peripheral blood BCAT greater than or equal to 1500TB/mm3 for at least 6 months) . Eosinophilic syndrome is a condition characterized by peripheral blood eosinophilia with organ system symptoms or dysfunctions directly related to eosinophilia. in the absence of parasitic infections, allergies, or secondary eosinophilic causes. Symptoms are variable, depending on which organs are dysfunctional. Diagnosis includes ruling out other causes of eosinophilia including bone marrow and genetic testing. Treatment usually begins with prednisone, and in a more common form is imatinib.
HES pathology was previously considered idiopathic, but is now known to be caused by various disorders, some of which have a known cause. A limitation of the traditional definition is that it does not include patients with a number of similar abnormalities (eg, chromosomal defects) that are known causes of HES but who do not respond. Traditionally defined HES in terms of degree or duration of eosinophilia. Another limitation is that in some patients eosinophilia and organ damage are characteristic features of HES. These patients need to be treated earlier than 6 months is required to confirm the diagnosis of HES.
HES pathology is rare, of unknown incidence, and usually occurs between the ages of 20 and 50 years. Only patients with persistent eosinophilia causing organ disturbances characterize the eosinophilic syndrome. Although any organ can be involved, it is mainly the heart, lungs, spleen, skin, and nervous system that are affected. Heart involvement can cause significant morbidity and mortality.
Subtypes
There are two subtypes:
Myeloproliferative variant Lymphocyte proliferative variant The myeloproliferative variant is usually associated with the loss of chromosome 4 at the CHIC2 site giving rise to the FIP1L1/ hybrid gene. PDGFRA (with tyrosine kinase activity that induces hematopoietic cell transformation). Patients usually have:
Splenomegaly, Thrombocytopenia, Anemia, Elevated serum vitamin B12 levels, Decreased eosinophils and vacuoles Myeloma Fibrosis Patients in this subgroup often develop cardiomyopathy and rarely progress. acute myeloid or lymphoid leukemia. Patients with the FIP1L1/PDGFRA transgene, usually male, may respond to low-dose imatinib (a tyrosine kinase inhibitor).
2.2. Infectious diseases:

Parasites are living organisms that are parasitic in hosts such as animals, livestock, poultry and in humans, they reproduce and grow rapidly, causing disease in the host. Parasites are of three main types:
Protozoa: protozoa, which reproduce and develop by division, duplication, and parasitism in the host body. Worms, flukes: they parasitize internal organs, visible to the naked eye. The parasitic worms in human internal organs such as roundworms, pinworms, liver flukes,... Ectoparasites: live parasitic outside the host body such as fleas, lice, lice,... Some Common diseases caused by parasites in humans: malaria, liver flukes, helminths, warts, sepsis, tapeworm infection with diphtheria,... and many other dangerous diseases.
To diagnose this pathology, it is necessary to take history, medical history, test for parasites in stool, serology test, treat parasites.
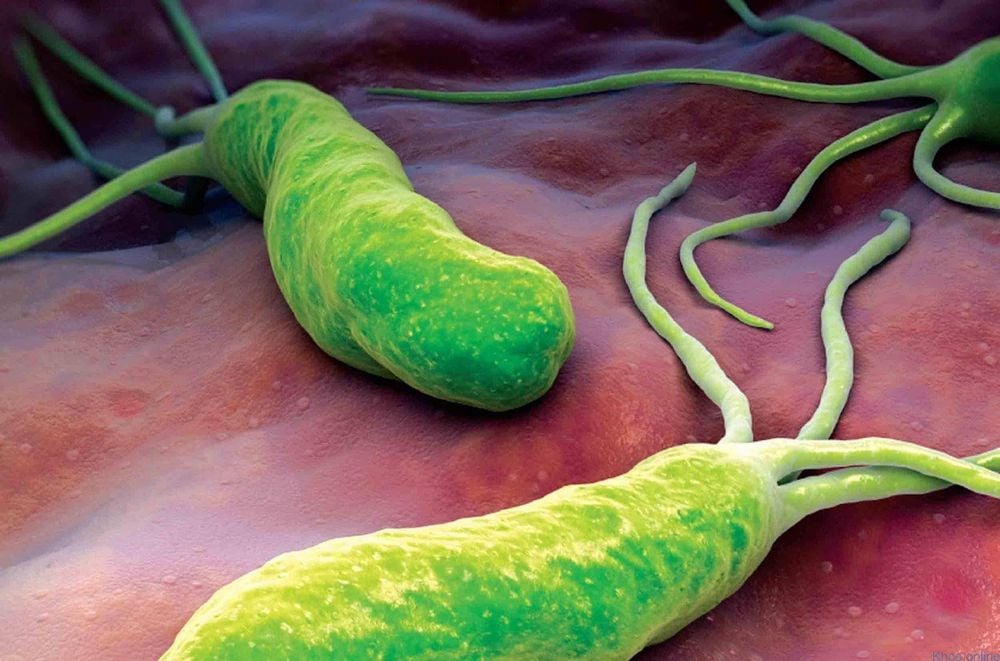
2.3. Helicobacter pylori, E.coli, Shigella Infection Helicobacter pylori, E.coli, Shigella infection can also cause gastrointestinal eosinophilia, gastric biopsy, stool test, stool culture, blood culture to diagnose this disease.
2.4. Using drugs such as antibiotics, NSAIDs... Using drugs such as antibiotics, NSAIDs... can also cause eosinophilia in the gastrointestinal tract, it is necessary to take careful history to confirm the diagnosis. guess.

2.5. Crohn's or hemorrhagic ulcerative colitis These conditions have similar clinical and histopathological symptoms such as eosinophilic colitis, need to perform gastroscopy, whole colon with biopsy , combined with the test of Anti-Saccharomyces cerevisiae antibodies, ANCA.
2.6. Celiac disease Celiac disease, also known as gluten intolerance, is a disease caused by a reaction to gluten, preventing the body from absorbing gluten-containing foods. Gluten are different proteins found in wheat and in other grains such as barley and rye.
Celiac disease leads to inflammation and aplasia of the lining of the small intestine causing a series of digestive disorders, reducing the ability to absorb nutrients in the small intestine.
The disease can occur at any age or may appear early in childhood and is often associated with other autoimmune diseases such as type 1 diabetes, autoimmune thyroiditis...
Usually the treatment of the disease Mainly dietary changes. It can be controlled by following a gluten-free diet, which means you don't eat any foods that contain gluten. The application of this diet can be troublesome, but if not adhered to, the disease can return and the patient at that time cannot be detected.
Diagnosis of this pathology should be based on abnormalities Anti-ransglutaminase antibodies, atrophy of duodenal villi...
2.7. Autoimmune diseases, vasculitis These diseases also cause eosinophilia in the gastrointestinal tract. Clinical examination should be combined with testing for ANCA antibodies and antinuclear antibodies.
2.8. Malignant pathology To diagnose this disease requires clinical examination, combined with imaging and biopsy as histopathology.
Eosinophilic gastroenteritis is a relatively rare chronic inflammatory disease, but its incidence has been underestimated. Because the clinical presentation of eosinophilic gastroenteritis lacks specificity, patients whose symptoms of chronic gastritis do not improve after repeated therapy should be examined such as endoscopy and histopathology to rule out eosinophilic gastroenteritis. The longer these symptoms last, the more likely the person is to develop eosinophilic gastroenteritis. Peripheral eosinophilia is not required for the diagnosis of eosinophilic gastroenteritis, and multiple site biopsies and microscopic eosinophil counts are more important. A good relationship between clinicians, endoscopists, and pathologists can help reduce the missed diagnosis rate of this disease.
Vinmec International General Hospital is a prestigious address trusted by many patients in performing diagnostic and treatment techniques for digestive diseases. Along with that, at Vinmec Hospital, the diagnosis of gastrointestinal diseases is done through gastroscopy and colonoscopy with Olympus CV 190 endoscope, with NBI (Narrow Banding Imaging - endoscopy) function. with narrow light spectrum) results in clearer mucosal pathological analysis results than conventional endoscopy, detection of inflammatory lesions, early gastrointestinal cancer lesions. Vinmec Hospital with modern facilities and equipment and a team of experienced experts who are always dedicated in medical examination and treatment, customers can rest assured with the gastrointestinal endoscopy service at the hospital. Vinmec International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.