This is an automatically translated article.
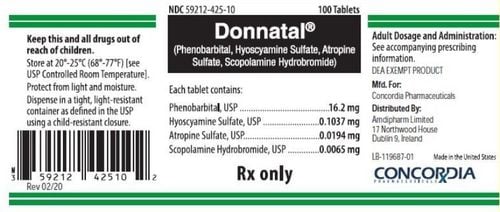
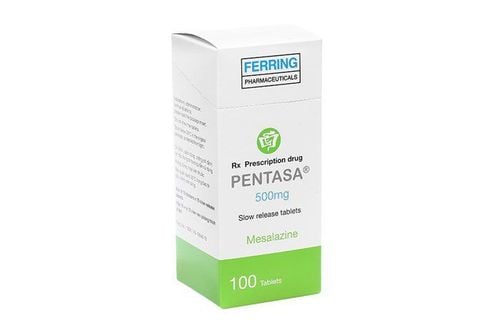
The article was written by Master - Doctor Mai Vien Phuong - Head of Gastrointestinal Endoscopy Unit - Department of Medical Examination and Internal Medicine - Vinmec Central Park International General Hospital.Ulcerative colitis (ulcerative colitis) is a chronic inflammatory condition of unknown etiology and with a relapsing clinical course. About half of the patients had a mild episode that was easily manageable with aminosalicylate, while the other half required at least one course of oral or intravenous corticosteroids.
Of the following drugs, immunosuppressants (including thiopurines and/or biologic agents) are required in 75% of cases for steroid refraction, steroid dependence, or chronic disease activity.
Even with the more potent drugs available, only 30% to 40% of those patients achieve adequate disease control (i.e. clinical remission) in the medium term as assessed in the randomized controlled trials (randomized controlled studies) and a large proportion of them lose out on long-term initial therapeutic benefit.
In addition, immunosuppressive drugs increase the risk of serious/opportunistic infections and cancer, as well as other adverse outcomes, such as exacerbation of chronic heart failure and other adverse events. thromboembolic complications, especially in elderly patients with elderly or long-standing onset, chronic ulcerative colitis, and those with other comorbidities.
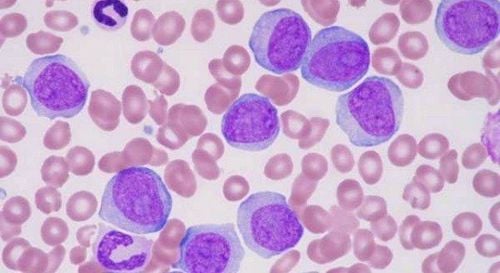
1. Modification of mucosal neutrophil activity and count may be a possible treatment in ulcerative colitis
From a pathogenic point of view, neutrophils appear to play an important role in tissue damage. As in other chronic inflammatory conditions, dysregulation of neutrophil apoptosis has been observed in ulcerative colitis. Neutrophil infiltration is a hallmark of ulcerative colitis as highlighted by the fact that it is an important component of the grading of ulcerative colitis severity in several histological scores.Furthermore, the presence of neutrophils in mucosal colonic biopsies is associated with the risk of clinical recurrence and even dysplasia, leading some authors to consider histological remission as a goal. Last resort in ulcerative colitis. Thus, modulating mucosal neutrophil activity and numbers could be a possible treatment in ulcerative colitis, although no drugs that target these cells are yet available.
Di chuyển bạch cầu hạt giúp điều trị viêm loét đại tràng
2. Therapeutic effect of granulocyte/monocyte migration method (GMA)
The therapeutic effect of granulocyte/monocyte migration (GMA) is based on the removal of activated neutrophils from the blood stream without increasing the risk of infection, since the cells are not Adults are migrated from the hematopoietic pools. In Japan, the granulocyte/monocyte migration method has been covered by the National Health Insurance for the treatment of active ulcerative colitis since April 2000 and it is widely used in clinical practice, even as first-line therapy for moderately to severely active ulcerative colitis in monotherapy.However, although the CE-marked granulocyte/monocyte migration method for the treatment of ulcerative colitis, Crohn's disease, pustular psoriasis and Behçet's disease is available in the European Union, it is almost Not used in Europe.
Other apheresis techniques that focus on the removal of lymphocytes have been studied in the past but they are not currently commercially available. Because several genetic, epidemiological and clinical differences between Western and Asian ulcerative colitis have been reported and these may lead to differences in response to therapies, The authors wish to provide an overview of the mechanism of action, recent clinical data and practical aspects of the use of GMA in ulcerative colitis from a European perspective.
3. Selective mechanism of action of granulocyte/monocyte migration method
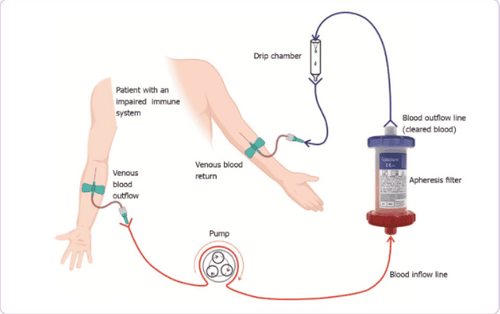
The granulocyte/monocyte migration method is an electrical technique that moves from a vein to a vein outside the body. The device for performing granulocyte/monocyte migration is available (Adacolumn TM, JIMRO, Takasaki, Japan) as a column containing 35,000 cellulose diacetate beads (2 mm diameter) as the method carrier. granulocyte/monocyte migration was immersed in isotonic saline in a 335 mL polycarbonate shell.Blood flows into the column and back to the patient via the column outlet, usually through two peripheral venous catheters. Numerous clinical, in vitro and ex vivo studies have been performed to determine the mechanism of action of the granulocyte/monocyte migration method. The main effect is the selective removal of granulocytes, monocytes, along with a smaller number of platelets from the blood stream, which can be seen by comparing their numbers in the inflow column and output line.
Cellulose granules absorb immunoglobulins (Ig) G and immune units in the circulation and trigger the activation of complement fragments C3a and C5a, allowing elimination of granulocytes and monocytes through the interaction of IgG and immunomodulatory monomers with the Fc gamma receptor and the binding sites of leukocyte complement, the receptor (not present in lymphocytes). Thus, granulocyte/monocyte migration method carriers selectively adsorb leukocytes from peripheral blood, with granulocytes exhibiting the highest affinity for the carrier particles.
Despite removal of granulocytes, the total circulating granulocyte count after granulocyte/monocyte migration method remained stable. In fact, flow cytometry studies in inflow and outflow column lines have observed a decrease in CD10(+) (mature and activation) and an increase in CD10(-) granulosa cells. (immature, unactivated), indicating an increase in the number of circulating cells.
Similarly, a significant decrease in peripheral CD14(+) and CD16(+) monocytes (proinflammatory phenotype) was observed in patients with inflammatory bowel disease treated with genetics. granulocyte/monocyte transfer. Finally, a significant increase in circulating levels of the CD4+CD25high+/FoxP3 phenotype (functional regulatory T cells) after a single course of granulocyte/monocyte migration therapy was also observed. reported in patients with ulcerative colitis.
Sơ đồ cơ bản của quy trình điện di chuyển bạch cầu hạt
| Trong bộ lọc hấp thụ | Trong máu của bệnh nhân |
| (1) Hấp thụ IgG lưu hành và các đơn giản miễn dịch bởi các hạt xenlulo; | (1) Giảm bạch cầu trung tính hoạt hóa và bạch cầu đơn nhân chống viêm (CD14 + CD16 +); |
| (2) Hoạt hóa các đoạn bổ thể (C3a, C5a); | (2) Tế bào apoptotic tương tác với tế bào B điều hòa, tạo ra IL-10 và tế bào B điều hòa trưởng thành; |
| (3) Hấp thu bạch cầu hạt và bạch cầu đơn nhân qua các thụ thể Fc𝛾 (IgG và immune complexes) và các vị trí liên kết của các thụ thể bổ thể bạch cầu (không có trong tế bào lympho); | (3) Sự trở lại của các chất do tế bào hấp phụ giải phóng: IL-1ra và HGF. |
| (4) Tạo ra tế bào apoptotic. |
In addition to these changes in peripheral leukocyte phenotypes, in vitro studies used whole blood of humans incubated with the medium. granulocyte/monocyte migration method measured significant amounts of interleukin (IL)-1 receptor antagonist, hepatocyte growth factor and soluble tumor necrosis factor (TNF) receptor I and II released from granulocytes and monocytes bound to the carrier.
Interestingly, the number of these anti-inflammatory cytokines is proportional to the number of cells that adhere to the carrier. Some of these cytokines can reach the patient's circulatory system, having a beneficial effect on the inflammatory process. Ultimately, exposure of neutrophils to cellulose granules results in the generation of apoptotic cells, and more than 40% of these apoptotic cells re-enter the patient's bloodstream and can interact with B cells. , induces IL-10 that produces regulatory B cells.
Above is some information about the method of granulocyte/monocyte migration in the treatment of ulcerative colitis. Please follow the website: Vinmec.com regularly to update many other useful information.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Domènech E, Grífols JR, Akbar A, Dignass AU. Use of granulocyte/monocyte apheresis in ulcerative colitis: A practical review from a European perspective. World J Gastroenterol 2021; 27(10): 908-918 [PMID: 33776362 DOI: 10.3748/wjg.v27.i10,908]