This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastroenterologist - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Autologous platelet-rich plasma as a shield against post-EMR (endoscopic mucosal resection) wounds in a preclinical model. Platelet-rich plasma injection solution has shown the best electrical and rheological properties for performing safe endoscopic resection.
1. Overview
Submucosal fluid injection is important to prevent late perforation (DP) in advanced resection techniques, endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD), by avoiding deep thermal injury. Perforation rates have traditionally been considered a quality of standard practice. It has a rate of 0.03%-0.8% in diagnostic procedures and 0.15%-3% in therapeutic procedures. On the other hand, late bleeding (DB) was the most worrisome and frequent side effect after these ablations, with an incidence of 2.6%–9.7 % not prevented by adding adrenaline to the buffer. submucosal or argon plasma ablation, because these methods only reduce the rate of premature bleeding.
There is no scientific evidence to recommend systematic prophylactic clipping to prevent late bleeding because they are ineffective in major mucosal defects and increase procedure costs. The ideal submucosal injection solution should provide long-term support, facilitate patch ablation, be inexpensive, be widely available, and have few side effects. The optimal fluid to lift the lesion is still a matter of debate. Autologous platelet-rich plasma as a shield against post-EMR (endoscopic mucosal resection) injuries in a preclinical model. Platelet-rich plasma injection solution has shown the best electrical and rheological properties for performing safe endoscopic resection.
2. Research results of platelet-rich plasma injection in endoscopic resection of large pedicleless lesions
A study was performed in the Department of Gastroenterology, Germans Trias University Hospital, Spain to prospectively evaluate the effect of platelet-rich plasma (PRP) submucosal injection on endoscopic resection. large sessile lesions.
A total of 11 cases of laparoscopic mucosal resection performed to treat large colorectal or gastric lesions were performed. There were 6 (54.5%) female and their mean age was 68.3 (53 to 84 years old). More than half were located in the rectum or left colon, the mean baseline platelet count was 175 × 10 9/L, while platelet-rich plasma obtained 2 times the baseline value. The mean lesion size was 46.4 mm (SD, 11.4 mm; range 40-70 mm). Complete resection was achieved in all cases. Histology revealed no deep submucosal invasion in all patients. Complications of late perforation or late bleeding were not observed in any of the cases. Platelet-rich plasma injection did not prolong the EMR time. No evidence of gastrointestinal narrowing was found during follow-up. The mean ulcer area at baseline was 22.7 cm2 ± 11.7 cm2 while after 4 weeks it was 2.9 cm2 ± 1.5 cm2. The rate of mucosal healing at week 4 was 87.5%.
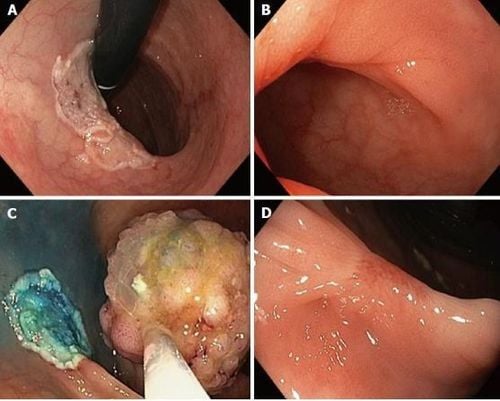
3. Mucosal healing after endoscopic resection in two patients treated with submucosal injection of platelet-rich plasma at baseline and after 4 weeks.
According to the study authors, platelet-rich plasma was obtained with the OLIN-1 kit (sterile disposable product), in both 20mL and 40mL formats, from a patient's blood sample (18-36mL) collected at endoscopic unit before performing EMR. Peripheral blood was centrifuged (2500 rpm/8 min at room temperature). Depending on the size of the lesion, smaller or larger than 40mm, the authors used 18 or 36 mL of blood (1 or 2 kits). A 20mL syringe filled with 2 mL of acid citrate dextrose (15% vol/volume) was used for standard blood collection. Syringes are centrifuged to obtain two different layers; RBCs (±45% volume) are placed at the bottom and platelet-rich plasma (55% volume, approximately 8mL) on top. Platelet-rich plasma was activated upon the addition of 20 mmol/L CaCl2 just before storage. A sample of 10 μL of blood and plasma was used to measure basal blood platelet counts and platelet-rich plasma platelet counts.4. The role of the submucosal method
In this prospective study, the authors found that submucosal injection of platelet-rich plasma demonstrated efficacy in the EMR of lesions larger than 35mm, showing potent healing activity. Otherwise, the use of a platelet-rich submucosal fluid buffer will prevent the incidence of late bleeding or late perforation. EMR and ESD are ablation techniques that can produce side effects, such as perforation or bleeding. Bleeding after EMR occurs in 5%-7% of lesions ≥ 20 mm, while perforation is an uncommon occurrence with an incidence of 1.4%-1.5%.
Elevation of the mucosa through the injection of solution into the submucosal space can reduce the rate of these events and improve the technical feasibility of the procedure. Normal saline is the most widely used solution but is not the most convenient for large lesions due to the maintenance of a fluid buffer. Accordingly, we should use other biocompatible lifting solutions that are easy to prepare and use. The use of platelet-rich plasma involves taking a sample of the patient's blood prior to the endoscopy procedure and concentrating the autologous platelets by centrifugation. Platelet-rich plasma fluid containing at least 2 times the peripheral blood platelet value and high levels of growth factors essential for mucosal healing, released from activated platelet alpha particles .
5. Rationale for the use of platelet-rich plasma
The rationale for using platelet-rich plasma to perform submucosal injection in endoscopic resection lies in the exponential release of multiple bioactive factors, followed by enhanced its natural healing process as well as its hemostatic properties, with a very low risk of scarring or severity.
In gastrointestinal disorders, platelet-rich plasma has proven effective in the prevention of delayed perforation and wound healing in primary colonic anastomosis. Previous reports have confirmed that platelet-rich plasma-enhanced surgical sites heal at two to three times the rate of untreated surgical sites and anabolic effects. directly related to platelet count.
6. Advantages of platelet-rich plasma injection in EMR
The authors' study examined the efficacy of platelet-rich plasma in the EMR of large lesions, obtained through an inexpensive kit, showing a strong anabolic effect. On the other hand, platelet-rich plasma has favorable biological and rheological properties compared with other solutions such as hyaluronic acid. This faster and stronger healing action acts as a mechanical defense, preventing the occurrence of delayed adverse events. Regarding late bleeding, platelet-rich plasma by mimicking the final step of the coagulation cascade, fibrin clot formation, submucosal injection develops a more stable shield against this complication.
7. Limitations of the study
The authors' study has some limitations because of the small number of patients, so larger studies are needed to perform a comparative study with other advanced solutions. Platelet-rich plasma is an readily available solution with favorable biological activities that has been shown to be administered as mucosal injection prior to endoscopic resection of large lesions. These data highlight the need for further research in this topic.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Lorenzo-Zúñiga V, de Vega VM, Bartolí R, Marín I, Caballero N, Bon I, Boix J. Submucosal injection of platelet-rich plasma in endoscopic resection of large sessile lesions. World J Gastrointest Endosc 2018; 10(11): 348-353 [PMID: 30487945 DOI: 10.4253/wjge.v10.i11,348]