This is an automatically translated article.
The article was written by Specialist Doctor I Tran Ngoc Thuy Hang - Resuscitation - Emergency Doctor - Emergency Resuscitation Department - Vinmec Central Park International General Hospital.
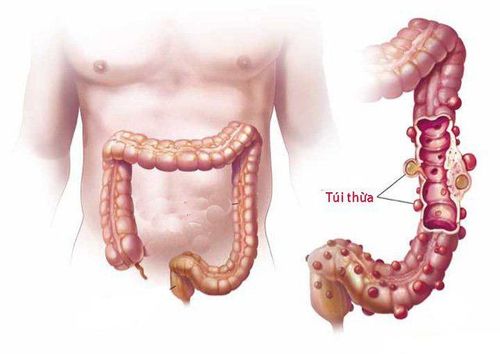
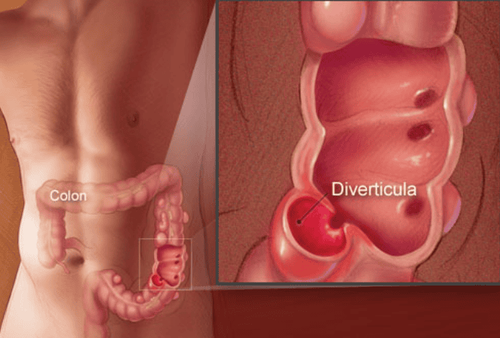
Diverticulitis, specifically colonic diverticulitis, is a digestive disease characterized by inflammation of abnormal pouches - diverticula - that can develop in the wall of the large intestine. Symptoms often include sudden onset of lower abdominal pain but onset can also occur within a few days.
1. Overview of colonic diverticulitis
Colonic diverticulum is a pouch-like protrusion from the intestinal wall. When one or more pouches become inflamed and, in some cases, infected, the condition is called diverticulitis. Complications of diverticulitis include abscess, inflammatory diverticulitis/perforation, intestinal obstruction, etc.
Approximately 20% - 50% of patients have recurrent diverticulitis. However, recurrent episodes of diverticulitis were not associated with a higher risk of complications compared with the initial episode. The risk of recurrence is higher in younger people and in women. Increasing age is associated with a higher risk of systemic and local complications per decade. A small number of patients following an episode of acute diverticulitis may develop segmental colitis associated with inflammatory diverticulitis, which is characterized by inflammation similar to inflammatory bowel disease.
Recurrent episodes of acute diverticulitis or persistent inflammation can lead to fibrosis and progressive scarring, leading to narrowing of the colon. Patients with colonic stenosis may present with symptoms of dull abdominal pain and constipation or acute intestinal obstruction without diverticulitis.
Mortality in patients with acute diverticulitis varies depending on the presence of complications and the patient's comorbidities. In patients with uncomplicated acute diverticulitis, conservative treatment is successful in 70% to 100% of patients and mortality is negligible. In patients with complicated diverticulitis who have undergone a single surgery, the mortality rate is approximately 0.6% to 5%. Mortality is up to 20% in patients with purulent diverticulitis or fecal peritonitis.
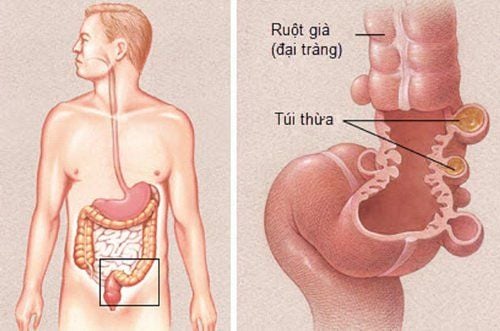
Khi một hoặc nhiều túi thừa bị viêm và trong một số trường hợp bị nhiễm trùng, tình trạng đó được gọi là viêm túi thừa.
2. Manifestations of colonic diverticulitis
The clinical presentation of the disease depends on the inflammatory process and associated complications:
Abdominal pain: is the most common complaint in patients with diverticulitis. The most common site of pain is the left lower quadrant in relation to the sigmoid colon, however, patients may complain of pain in the right lower quadrant or suprapubic region (also associated with sigmoid diverticulitis). ), less commonly cecal diverticulitis. Approximately 20% of patients with a previous episode of acute diverticulitis report chronic abdominal pain. In some patients, it may be due to irritable bowel syndrome. However, in about 5% of patients, chronic abdominal pain is caused by mild or insidious diverticulitis with persistent chronic diverticulitis.
Nausea and vomiting are reported in 20% to 62% of patients related to peritoneal irritation and bowel obstruction. The patient may also have a low-grade fever. In case of colonic diverticulitis with complications of perforation, peritonitis can cause shock and hypotension. Physical examination may reveal local peritoneal signs such as local resistance, abdominal distension, and rebound tenderness. Rectal examination may reveal a mass or resistance when there is an abscess in the distal sigmoid colon, and bloody stools are withdrawn. Diverticulitis may be associated with changes in bowel habits such as constipation in 50% of patients and diarrhea in 25%-35% of patients. 10%-15% of patients with acute diverticulitis present with urinary disturbances such as urgency, frequency, or urinary retention. 25% of patients with acute diverticulitis have acute or chronic complications such as:
Abscess: Diverticulitis occurs in about 17% of patients hospitalized for acute diverticulitis. Symptoms of diverticulitis are similar to those of acute diverticulitis. Diverticulitis may be noted on contrast-enhanced CT of the abdomen. Therefore, a diverticulum abscess should be suspected in patients with diverticulitis who do not improve with persistent abdominal pain or fever despite 3 days of antibiotic therapy. Rarely, patients may develop a pyogenic liver abscess due to the spread of the infection through the portal circulation. Intestinal Obstruction: During an acute episode of diverticulitis, partial obstruction of the colon may occur due to relative stricture due to diverticulitis or a compressing diverticulum abscess. However, severe colonic obstruction rarely occurs in the acute phase and is often associated with later development caused by strictures due to chronic diverticulitis. Acute diverticulitis can also cause small bowel obstruction if a loop of the small intestine is attached to a diverticulitis-peritoneal mass. Depending on the degree and location of the obstruction, the patient may experience abdominal pain, nausea, vomiting, abdominal distension, and bowel obstruction. Patients with semi-obstruction or intestinal obstruction may have abdominal distention, cramping pain, resounding abdominal percussion, bowel movements may be increased by the obstruction or decreased in the case of paralytic ileus.
Colonic fistula: The inflammation caused by acute diverticulitis can lead to the formation of a fistula between the colon and adjacent organs. The fistula usually involves the bladder. Patients with colic-bladder fistula may present with hematuria, hematuria, or dysuria. Patients with colo-vaginal fistula may see gas and stool in the vagina. Perforation: Perforation due to generalized peritonitis can result from rupture of a diverticulum abscess into the peritoneal cavity or rupture of an inflamed diverticulum with fecal contamination of the peritoneum. Although only 1% to 2% of patients with acute diverticulitis perforate with purulent or fecal peritonitis, mortality is as high as 20% in patients with perforated diverticulitis with peritonitis. diffuse, abdominal distension, abdominal wall resistance, bowel motility loss.

Đau bụng là dấu hiệu than phiền thường gặp nhất ở các bệnh nhân viêm túi thừa đại tràng.
Subclinical manifestations:
Blood tests show an increased inflammatory index: Including a blood count test, white blood cells are increased, CRP and procalcitonin are increased. Other tests help in supportive assessment and rule out other causes: Urea, creatinine, electrolytes, serum aminotransferase, alkaline phosphatase, bilirubin, amylase and lipase,... Pregnancy testing should be done in all women women of reproductive age. Urinalysis: Sterile pyuria may be seen due to adjacent inflammation. The presence of colonic resident microbiota on urine culture suggests a colostomy-vesical fistula. Imaging:
Contrast-enhanced computed tomography (CT) of the abdomen: Presence of local intestinal wall thickening (> 4 mm), an increase in soft tissue density in peritoneal fat secondary to inflammation or fatty infiltration and colonic diverticulum. The sensitivity and specificity of abdominal CT for the diagnosis of acute diverticulitis are 94% and 99%, respectively. Complications of diverticulitis can also be detected on abdominal CT scans: Abscesses are defined as fluid collections surrounded by an area of inflammatory changes. The center of the collection area may contain vapor, fluid-vapor levels, or low-density tissue showing necrotic debris. On abdominal CT in patients with complications of intestinal obstruction due to acute diverticulitis, the presence of dilated loops of bowel with air-fluid levels near the area of fatty infiltration, inflammatory diverticulum was noted. The slightly free image in viscera other than the intestine in the abdomen suggests a colonic fistula complication. In patients with peritonitis, free abdominal air suggests fistula or perforation of an inflamed diverticulum. Abdominal ultrasound features suggestive of acute diverticulitis include: Hypoechoic diverticulitis reaction. Diverticular, peritoneal abscess formation with or without air bubbles. Intestinal wall thickening (intestinal wall thickness > 4mm) at the point of greatest pain. The presence of a diverticulum in the adjacent bowel. Complications of diverticulitis can also be detected by ultrasound. Abscesses appear as an anechoic mass containing echogenic debris. Features suggestive of a fistula include the presence of a hypoechoic area with air bubbles adjacent to the inflamed diverticulum extending to the bladder, vagina, or abdominal wall. In patients with peritonitis, diffuse peritoneal thickening, focal or generalized fluid collection may be seen. Ultrasound has the advantage of low cost, avoiding radiation exposure. However, it is highly operator-dependent and does not distinguish between other causes of abdominal pain.
Magnetic resonance imaging (MRI): Imaging findings suggestive of acute diverticulitis include colonic wall thickening, presence of diverticula, edema, and fluid between bowel loops. Nonspecific findings that may be seen on MRI include segmental colonic stenosis, ascites, and abscesses. Abdominal and chest radiographs: Nonspecific abnormalities seen on abdominal radiographs account for 30% to 50% of patients with acute diverticulitis. Manifestations include an air-fluid level in the bowel loops, a slightly dilated loop suggestive of intestinal obstruction or paralytic ileus, and increased soft tissue density suggestive of an abscess. An upright chest x-ray can detect free abdominal air with a crescent of air below the diaphragm in 3% to 12% of patients with acute diverticulitis. Note: Colonoscopy has no role in the diagnosis of acute diverticulitis. Colonoscopy should be avoided during the acute inflammatory phase because of the risk of perforation and progressive infection. After complete resolution of symptoms associated with acute diverticulitis (usually within 6 to 8 weeks), a screening colonoscopy can be performed.
3. Diagnosis
The diagnosis of acute diverticulitis should be considered in a patient with lower abdominal pain and abdominal wall reaction on physical examination. The pain is usually in the left quadrant, however, it can be in other locations. A blood test for CRP leukocytosis (>50mg/dL), although not sensitive or specific for acute diverticulitis, can support the diagnosis. On imaging, computed tomography of the abdomen with contrast is best to confirm the diagnosis of acute diverticulitis.
Differential diagnosis:
Irritable bowel syndrome (IBS): Abdominal discomfort in patients with IBS may be similar to that in patients with diverticulitis. However, symptoms of abdominal pain and changes in bowel habits are chronic in IBS patients. Patients with IBS often also have symptoms of gas, bloating, diarrhea, and/or constipation. Colorectal cancer: Patients with colorectal cancer and acute diverticulitis may present with similar clinical presentations and are shown to have thickened colonic wall on CT. However, the presence of inflammation of the bowel wall and mesentery of the colon greater than 10 cm and the absence of lymph node enlargement on abdominal CT strongly suggests acute diverticulitis. In 10%-20% of patients, it is difficult to distinguish between acute diverticulitis and colorectal cancer on abdominal CT scan, and colorectal cancer can only be ruled out by colonoscopy after resolution of the acute inflammation. count. Acute appendicitis: Common symptoms of appendicitis include right lower abdominal pain, loss of appetite, fever, nausea, and vomiting. Abdominal pain initially in the epigastrium, later, spreading to the right iliac fossa. Abdominal CT scans can differentiate between acute appendicitis and acute diverticulitis. Inflammatory bowel disease: In patients with inflammatory bowel disease, the main symptom is diarrhea instead of abdominal pain. In addition, the patient had symptoms for several months prior to presentation. Although abdominal CT can show wall thickening in both acute diverticulitis and colitis, the presence of diverticulum and diverticulitis is indicative of acute diverticulitis. Infective colitis - diarrhea is the predominant symptom. The patient may have a history of previous antibiotic use or recent travel. Stool culture can identify pathogens. Ischemic colitis: Patients with ischemic colitis often present with rapid-onset abdominal pain, bloody stools, or bloody diarrhea. Patients may have risk factors for ischemic colitis (>60 years of age, hemodialysis, hypertension, diabetes mellitus, dehydration, or laxative use). Abdominal CT can show segmental thickening, similar to a patient with acute diverticulitis, but without the presence of an inflamed diverticulum. Other differential diagnoses include tubal abscess, ovarian cyst, ovarian torsion, ectopic pregnancy, cystitis, and nephrolithiasis. The differential diagnosis is based on history, physical examination, and laboratory findings.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.