This is an automatically translated article.
Posted by Dr. Truong Ngoc Hai - Resuscitation Doctor - Emergency Department - Vinmec Central Park International General Hospital
Invasive Candida infections are one of the major causes of morbidity and mortality in humans, causing a wide spectrum of clinical pathology: from superficial, superficial fungal infections to other conditions. invasive conditions such as fungal infections of the blood and involvement of distant organs (eyes, heart valves, kidneys...).
1. Overview of what is candida infection?
At the end of the 20th century, Candida strains were considered the most common fungal pathogens in the human body and into the 21st century, this is still recognized although many new groups of agents are gradually emerging. Candida has approximately 150 different strains that grow mainly in single-celled “yeast” forms, with a few strains being able to grow in other forms such as “pseudohyphae” (pseudomycelium) and “hyphae” (eg. example: Candida albicans). Candida spp. found in a wide variety of environments, including a small number of strains associated with colonization and disease in humans.
Classification of fungi according to biological characteristics:
Yeast (cell fungi): resembling round cells (Candida, Cryptococcus). Mycelium (mold): mycelium in the infected tissue (Aspergillus, Zygomycetes). Dimorphic fungi: like yeast when in tissue or culture at 370C, but have a filamentous structure in normal media (Coccidioides, Histoplasma). Yeast species can be either facultative aerobic or facultative anaerobes. In the absence of O2, yeasts generate energy by converting carbohydrates into CO2 and ethanol or lactic acid.
Yeast can reproduce asexually through budding or sexually through the formation of sporangia. During asexual reproduction, a new bud develops from the parent yeast when conditions are right, after the bud reaches the size of a mature yeast, it separates from the parent yeast. When nutritional conditions are poor, yeasts capable of sexual reproduction produce sporangia.
According to experts, there are 2 types of yeast:
Genuine yeast: reproduces by means of the ascus, typically Saccharomyces yeast. Yeast without cysts: constitutes a large family Cryptococcacea and Candida is one of the species in the family Cryptococcacea. Candida infections (mostly Candida albicans) can cause acute, subacute, or chronic disease. In which, mucosa and skin are the most commonly injured sites, sometimes fungi cause sepsis, endocarditis and meningitis. Visceral candidiasis is common in patients with impaired cell-mediated immunity and in patients undergoing cancer treatment, immunosuppressive therapy, or anti-rejection therapy.
Candida albicans is a round or oval yeast about 2-5 μm in size, living normally in the intestines of humans and many mammals (endophytic). In healthy individuals, Candida spp. Found in mouth 30%, intestines 38%, vagina 39%, perianal skin folds 46%, bronchi 17%.
In the saprophytic state, the number of fungi is very small, fresh examination of biological fluids from the mucosa rarely shows one or two budding yeast granulosa cells. Here, the fungus maintains a balance with the bacteria that live with it, all of which constitute the body's normal flora. A healthy gut usually has about 1000 bacteria and 1 Candida yeast cell. This bacteria keeps the Candida fungus “in check” and prevents it from becoming mycelium (chronic invasive fungal form). When the balance is disturbed by antibiotics, the beneficial bacteria in the gut (Lactobacillus acidophillus and Bifidobacteria) die. At this time, Candida yeast (not affected by antibiotics) will proliferate and spread rapidly in the human body.

Sợi tơ nấm Candida (nhiễm Candida mạn tính)
Under certain conditions, Candida spp. transition from a saprophytic state to a parasitic (pathogenic) state. Characteristic of the parasitic state is the greatly increased number of fungi, the formation of pseudohyphae, which allows the fungus to crept between the host cells and penetrate deeper. Conditions favorable for Candida spp. Pathogenicity is =:
Physiological factors: when a woman is pregnant, an increase in hormones leads to ecological changes in the vagina (sweet biological fluid, glycogen storage in epidermal cells), plus immunosuppression makes fungal growth more favorable.
Pathological factors: immunodeficiency, diabetes, obesity, malnutrition ...
Occupational factors: Frequent exposure to a humid environment can easily lead to dermatitis, inflammation of the nails and around the nails caused by Candida spp.
Drug factor:
Broad-spectrum antibiotics, using high doses and for a long time will kill bacteria that live with fungi. Thus disrupting the ecological balance in place. Corticosteroids: long-term use will reduce cell-mediated immunity. Immunosuppressive drugs: used in cancer treatment or therapy. Candidiasis is ubiquitous, with patients of all ages, races, and sexes. Accordingly, candidiasis can occur in any organ in the body, but the most common is still the skin and mucous membranes.
Diseases of the mucosa: thrush (thrush), esophagitis, enteritis, vaginitis-vulva, anal and perianal inflammation. Diseases of the skin and adjacent organs: dermatitis, granulomatous dermatitis, inflammation of the nail and around the nail. Visceral disease: endocarditis (must have 3 factors: existing valvular disease, antibiotic use, opening for Candida spp. to enter the bloodstream), respiratory candidiasis, urinary tract disease, disseminated candidiasis (the first stage is a blood fungal infection, then the fungus invades multiple organs at once).
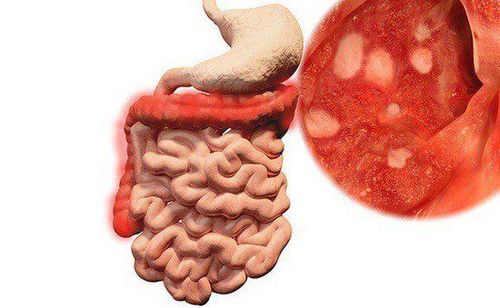
Bệnh vi nấm Candida có thể xảy ra ở niêm mạc viêm ruột
2. An overview of invasive candidiasis
Definition:
Fungal blood infection is the presence of fungi in the blood. Invasive fungal infection is the spread of fungi through the bloodstream to organs in the body such as eyes, heart valves, kidneys... Infection by Candida spp. It is one of the major causes of morbidity and mortality in humans, causing a wide spectrum of clinical pathologies: from superficial, superficial fungal infections to invasive conditions such as bloodstream infections. and affects distant organs (eyes, heart valves, kidneys...).
Candida is the causative agent of 70-90% of invasive fungal infections (1). In patients with sepsis, Candida is the 4th leading causative agent in the United States and the 7th in Europe (2, 3). A recent multicenter point-prevalence survey found Candida strains to be the most isolated healthcare-associated bacteremia agent. The frequency of Candida bacteremia is 0.5-1.4/10,000 patient-days of hospital stay (3, 4). The frequency of Candida bacteremia in the ICU is approximately 2/1000 ICU admissions (5, 6).
Candida enters the bloodstream via 3 routes:
From the intestine through the gastrointestinal mucosal barrier, this is the most common mechanism, immunocompromised patients and ICU patients have an overgrowth of Candida in the intestinal lumen. . Through an intravascular catheter. From an infection such as pyelonephritis. 2 groups of patients at high risk for Candida bacteremia:
Patients in the ICU. Immunocompromised patients. Risk factors in ICU patients
Elderly. Trauma, burns, abdominal surgery, gastrointestinal perforation, gastrointestinal junction fistula. Place a central venous catheter. Complete parenteral nutrition. Use broad-spectrum antibiotics. High APACHE II score. Among patients with candidemia and invasive candidiasis, non-albicans Candida strains account for approximately 50%. There are 15 strains of Candida that cause disease in humans, more than 90% of which are caused by the 5 most common strains: C.albicans , C.glabrata , C.tropicalis , C.parapsilosis and C.krusei .
Candidemia is associated with 47% of deaths (2, 4, 7-9) and is even higher in septic shock (10). Many authors suggest that mortality is related to timing of treatment and/or source control (10-15). Therefore, early intervention with appropriate antifungal therapy and removal of central catheters and infected materials generally contributes to improved prognosis for patients.
Central venous catheters are often associated with candidaemia, but catheters are not always a source of infection, especially in patients with agranulocytosis where the gastrointestinal tract is a common source of infection. Many experts agree that careful management of central venous catheters in particular patient populations is of great significance in the overall management of infections (15).
Blood cultures have poor diagnostic sensitivity, so this test remains a major barrier to early intervention of fungal infections. The development of highly reliable nonculture assays for early intervention and targeted antifungal therapy compared with traditional blood cultures is less sensitive and responds late.
Echinocandin is the first choice in the treatment of candidaemia and invasive candidiasis (except fungal infections of the central nervous system, eyes, urinary tract). Because of its safety, convenience, early fungicide, improved prognosis, and increased incidence of azole-resistant Candida strains (15, 16).
In summary, the current challenging and invasive fungal infections are:
Broad spectrum of pathogens: from superficial and mucosal infections to blood, deep tissue and organ infections. Blood fungal infections: increased mortality by 35-75%. Statistics in the United States: fungal blood infections are the 4th leading cause of healthcare-associated infections. ICU patients: more than 50% of patients have candidiasis at multiple sites, and 17% of ICU-acquired infections are caused by Candida. Diagnosis of invasive fungal infections is difficult. 70% of antifungal treatment in the ICU is empiric or directed. Meanwhile, late treatment significantly increases mortality.
Kollef et al showed that each hour of delay in giving appropriate antifungals reduced survival by 7.6% (10).
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
REFERENCES
Lamagni T, Evans B, Shigematsu M, Johnson E. Emerging trends in the epidemiology of invasive mycoses in England and Wales (1990–9). Epidemiology & Infection. 2001;126(3):397-414. Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB. Nosocomial blood infections in US hospitals: analysis of 24,179 cases from a prospective quality surveillance study. Clinical infectious diseases. 2004;39(3):309-17. Marchetti O, Bille J, Fluckiger U, Eggimann P, Ruef C, Garbino J, et al. Epidemiology of candidemia in Swiss tertiary care hospitals: secular trends, 1991–2000. Clinical Infectious Diseases. 2004;38(3):311-20. Gudlaugsson O, Gillespie S, Lee K, Berg JV, Hu J, Messer S, et al. Attributable mortality of nosocomial candidemia, revisited. Clinical Infectious Diseases. 2003;37(9):1172-7. Charles PE, Doise JM, Quenot JP, Aube H, Dalle F, Chavanet P, et al. Candidemia in critically ill patients: difference of outcome medical and surgical patients. Intensive care medicine. 2003;29(12):2162-9. Nolla-Salas J, Sitges-Serra A, Leon-Gil C, Martinez-Gonzalez J, Leon-Regidor M, Ibán P, et al. Candidemia in non-neutropenic critically ill patients: analysis of prognostic factors and assessment of systemic antifungal therapy. Intensive care medicine. 1997;23(1):23-30. Pappas PG, Rex JH, Lee J, Hamill RJ, Larsen RA, Powderly W, et al. A prospective observational study of candidemia: epidemiology, therapy, and implications on mortality in hospitalized adult and pediatric patients. Clinical Infectious Diseases. 2003;37(5):634-43. Pfaller M, Neofytos D, Diekema D, Azie N, Meier-Kriesche H-U, Quan S-P, et al. Epidemiology and outcomes of candidemia in 3648 patients: data from the Prospective Antifungal Therapy (PATH Alliance®) registry, 2004–2008. Diagnostic microbiology and infectious disease. 2012;74(4):323-31. Diekema D, Arbefeville S, Boyken L, Kroeger J, Pfaller M. The changing epidemiology of healthcare-associated candidemia over three decades. Diagnostic microbiology and infectious disease. 2012;73(1):45-8. Kollef M, Micek S, Hampton N, Doherty JA, Kumar A. Septic shock attributed to Candida infection: importance of empiric therapy and source control. Clinical infectious diseases. 2012;54(12):1739-46. Grim SA, Berger K, Teng C, Gupta S, Layden JE, Janda WM, et al. Timing of susceptibility-based anti drug administration in patients with Candida blood infection: correlation with outcomes. Journal of antimicrobial chemotherapy. 2011;67(3):707-14. Ostrosky-Zeichner L, Kullberg BJ, Bow EJ, Hadley S, León C, Nucci M, et al. Early treatment of candidemia in adults: a review. Medical mycology. 2011;49(2):113-20. Morrell M, Fraser VJ, Kollef MH. Delaying the empiric treatment of Candida blood infection until positive blood culture results are obtained: a potential risk factor for hospital mortality. Antimicrobial agents and chemotherapy. 2005;49(9):3640-5. Garey KW, Rege M, Pai MP, Mingo DE, Suda KJ, Turpin RS, et al. Time to initiation of fluconazole therapy mortality in patients with candidemia: a multi-institutional study. Clinical infectious diseases. 2006;43(1):25-31. Andes DR, Safdar N, Badley JW, Playford G, Reboli AC, Rex JH, et al. Impact of treatment strategy on outcomes in patients with candidemia and other forms of invasive candidiasis: a patient-level quantitative review of randomized trials. Clinical infectious diseases. 2012;54(8):1110-22. Mora-Duarte J, Betts R, Rotstein C, Colombo AL, Thompson-Moya L, Smietana J, et al. Comparison of caspofungin and amphotericin B for invasive candidiasis. New England Journal of Medicine. 2002;347(25):2020-9.