This is an automatically translated article.
Posted by Dr. Truong Ngoc Hai - Resuscitation Doctor - Emergency Department - Vinmec Central Park International General Hospital
The frequency of distribution of pathogenic Candida strains varies by region, between centers and even between units. Indeed, Candida infection is not one but many different disease states, with each Candida strain presenting with its own unique characteristics in terms of histotropy, propensity to invasive disease, toxicity, and drug susceptibility. . A solid understanding of local epidemiology and resistance will help make more informed treatment decisions while awaiting culture and antifungal results.
1. Distribution of Candida strains among regions
Population-based studies in Europe and the United States show that approximately 95% of candidaemia is caused by the following four strains: C.albicans , C.glabrata , C.parapsilosis and C.tropicalis . In which, C.albicans accounted for about 45-60% of all samples isolated from blood, followed by C. glabrata strain (18). In contrast, based on single-country studies, C.tropicalis appears to be predominant in Latin America as well as in Southeast Asia (19-21). However, these data are based on reports from small studies, with different methods of testing for antifungals. In particular, most of the published data is reported from Singapore, Thailand and Korea. Therefore, there is a gap in knowledge and expertise compared to other countries in the Asia-Pacific region.
Knowledge of the epidemiology of Candida strains is important when considering treatment, because susceptibility to fluconazole can often be predicted by identification of the causative organism. C.albicans generally responds to fluconazole, but natural resistance to fluconazole has recently been reported to be increased in C.glabrata , C.tropicalis (22) and C.parapsilosis (23) strains.
Susceptibility to fluconazole in the same Candida strain has been reported to vary from country to country or within countries, underscoring the importance of knowledge of the epidemiology and drug response in each country. local. Antifungal testing is not routinely performed in hospitals in the Asia-Pacific region. Clinicians often prescribe drugs empiric or based on response data from elsewhere, which is not applicable to the local epidemiology.
To complete the data for each region, a prospective, multicenter observational study was conducted across 13 centers in the Asia-Pacific region, over a 2-year period (2013-2015) and included A total of 861 Candida samples were isolated.
Table 1 - Distribution of Candida strains in the participating countries (17)
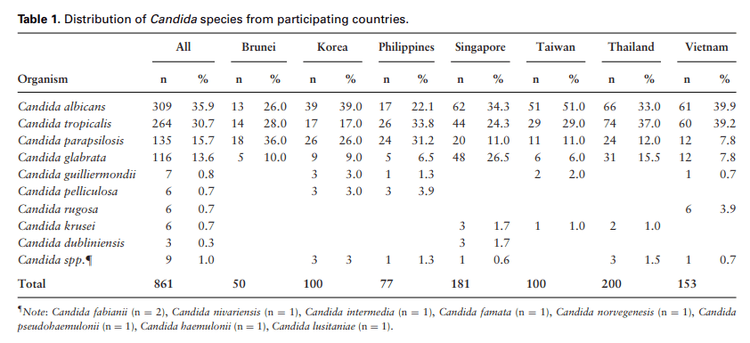
Bảng 1 - Phân bố các chủng Candida tại các nước tham gia nghiên cứu (17)
Research results on the distribution of Candida strains showed that the 4 most common strains were C.albicans (35.9%), C.tropicalis (30.7%), C.parapsilosis (15.7%) and C.glabrata (13.6). %).
C.albicans is the most common strain at centers in Korea, Singapore, Taiwan and Vietnam. C.tropicalis is common in centers in the Philippines and Thailand, while C.parapsilosis is most common in Brunei. It is worth noting that the proportion of non-albicans strains recorded was higher than that of C.albicans in most countries, except Taiwan.
In Vietnam, 6 common Candida strains are C.albicans (39.9%), C.tropicalis (39.2%), C.parapsilosis (7.8%), C.glabrata (7.8%), C.rugosa (3.9%). and C.guilliermondii (0.7%). In which, non-albicans strains accounted for 60.1%.
Table 2 - Antifungal susceptibility of the countries participating in the study( 17 )
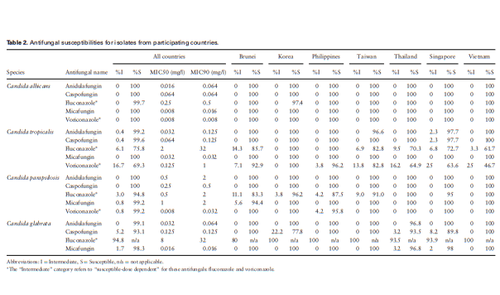
Bảng 2 - Tính nhạy cảm thuốc kháng nấm của các nước tham gia nghiên cứu(17)
C.albicans is also sensitive to fluconazole (99.7%). This susceptibility was lower in non-albicans strains, especially C.tropicalis (S=75.8%, S-DD= 6.1%, R=18.2%), C.glabrata (S-DD= 94.8%, R) = 5.2%) and C.parapsilosis (S= 94.8%, S-DD = 3% R=2.2%). There were regional differences in fluconazole susceptibility among non-albicans strains. C.tropicalis fluconazole resistance is highest in Thailand. (S=70.3%) and Vietnam (S=61.7%); meanwhile, fluconazole resistance of C. glabrata was highest in Brunei (S-DD= 80%) and Singapore (S-DD= 93.9%).
All isolated C.albicans samples were sensitive to voriconazole, but 16.7% of C.tropicalis had MICs in the S-DD range and 14% of C.tropicalis were resistant to voriconazole.
The activities of the 3 groups of echinocandins were still sensitive (S> 99%) to C.albicans, C.tropicalis and C.parapsilosis, but a small percentage of caspofungin resistance (low level) was observed. C.glabrata samples were isolated. A total of 12 isolates did not respond to caspofungin, of which 9 (75%) had MICs that fell into the intermediate response region. Resistance to caspofungin was most common in C. glabrata (n= 8) (S= 93.1%, S-DD= 5.2%, R= 1.7%), accounting for 62% of the total samples that did not respond. Most caspofungin unresponsive samples were tested for susceptibility to other echinocandins, because cross-resistance with any of the other two echinocandins was observed in only three strains (C.tropicalis, C.glabrata and C.krusei ). The gene mutations in the fks hotspot regions were identified in 2 isolates: C.glabrata (GenBank KT950827) and C.krusei (GenBank KT950828), and all 2 samples with the fks mutation showed cross-resistance with fks. at least 2 out of 3 echinocandins. The sensitivity to caspofungin was lowest in C. glabrata isolates from Korea (S= 77.8) and Singapore (S= 89.8%); however, the number of isolates with caspofungin resistance is not much.
There is no CLSI breakpoint for amphotericin B's antifungal activity against Candida strains. However, the MIC distribution range of amphotericin B against C.albicans (range 0.12-1.0 mg/l, MIC50 and MIC90= 0.5mg/l), C.tropicalis (0.25-1.0 mg/l, MIC50 and MIC90= 1.0 mg/l), C.parapsilosis (0.25-1.0 mg/l, MIC50= 0.5, MIC90= 1.0 mg/l) and C.glabrata (0.25-2.0 mg/l, MIC50 and MIC90= 1.0 mg/l) falls into the “wild-type” MIC distribution (24).
The results from this study are important for two reasons:
First, we found non-albicans strains to be the most frequent in the isolates from most cases of bacteremia in the pharynx. most of the countries in the Asia-Pacific region and of these, C.tropicalis and C.parapsilosis stand out.
Second, a significant proportion of C.tropicalis (and subsequently C.parapsilosis ) showed decreased susceptibility to fluconazole. It is implied that susceptibility to fluconazole in these non-albicans strains cannot be accurately predicted (25). These findings suggest that in the Asia-Pacific region, echinocandins should be selected in clinically unstable situations and in high-risk patients, with evidence of candidaemia (26). Routine antifungal treatment of non-albicans strains is recommended for appropriate use of azoles (27) and if fluconazole is considered empiric, then therapeutic dosing strategies should be implemented. appropriate treatment (28).
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
REFERENCES
Tan TY, Hsu LY, Alejandria MM, Chaiwarith R, Chinniah T, Chayakulkeeree M, et al. Antifungal susceptibility of invasive Candida blood isolates from the Asia-Pacific region. Sabouraudia. 2016;54(5):471-7. Hajjeh RA, Sofair AN, Harrison LH, Lyon GM, Arthington-Skaggs BA, Mirza SA, et al. Incidence of blood infections due to Candida species and in vitro susceptibilities of isolates collected from 1998 to 2000 in a population-based active surveillance program. Journal of clinical microbiology. 2004;42(4):1519-27. Colombo AL, Nucci M, Salomão R, Branchini MLM, Richtmann R, Derossi A, et al. High rate of non-albicans candidemia in Brazilian tertiary care hospitals. Diagnostic microbiology and infectious disease. 1999;34(4):281-6. 20. Foongladda S, Sakulmaiwatana P, Petlum P, Vanprapar N. Candida species, genotypes and antifungal susceptibility of Candida isolates from blood samples of patients at the largest tertiary care hospital in Thailand during 1999-2002. Journal of the Medical Association of Thailand= Chotmaihet thangphaet. 2004;87(1):92-9.
21. Tan TY, Tan AL, Tee NW, Ng LS, Chee CW. The increased role of non-albicans species in candidaemia: results from a 3-year surveillance study. Mycoses. 2010;53(6):515-21.
22. Kothavade RJ, Kura M, Valand AG, Panthaki M. Candida tropicalis: its prevalence, pathogenicity and increasing resistance to fluconazole. Journal of medical microbiology. 2010;59(8):873-80.
23. Pfaller MA, Jones RN, Castanheira M. Regional data analysis of Candida non-albicans strains collected in United States medical sites over a 6-year period, 2006–2011. Mycoses. 2014;57(10):602-11.
24. Pfaller MA, Espinel-Ingroff A, Canton E, Castanheira M, Cuenca-Estrella M, Diekema DJ, et al. Wild-type MIC distributions and epidemiological cutoff values for amphotericin B, flucytosine, and itraconazole and Candida spp. as determined by CLSI broth microdilution. J Clin Microbiol. 2012;50(6):2040-6.
25. Pfaller MA, Moet GJ, Messer SA, Jones RN, Castanheira M. Geographic variations in species distribution and echinocandin and azole antifungal resistance rates among Candida blood infection isolates: report from the SENTRY Antimicrobial Surveillance Program (2008 to 2009). Journal of clinical microbiology. 2011;49(1):396-9.
26. Hsueh P-R, Graybill JR, Playford EG, Watcharananan SP, Oh M-D, Ja'alam K, et al. Consensus statement on the management of invasive candidiasis in Intensive Care Units in the Asia-Pacific Region. International journal of antimicrobial agents. 2009;34(3):205-9.
27. Shah D, Yau R, Weston J, Lasco T, Salazar M, Palmer H, et al. Evaluation of antifungal therapy in patients with candidaemia based on susceptibility testing results: implications for antimicrobial stewardship programmes. Journal of antimicrobial chemotherapy. 2011;66(9):2146-51.
28. Clancy CJ, Victor LY, Morris AJ, Snydman DR, Nguyen MH. Fluconazole MIC and the fluconazole dose/MIC ratio correlate with therapeutic response among patients with candidemia. Antimicrobial agents and chemotherapy. 2005;49(8):3171-7.