This is an automatically translated article.
Metformin is a Biguanide group of antidiabetic drugs being used a lot today. Therefore, it is very important to understand and use this medicine correctly.1. Biguanide drug group (Metformin)
Metformin is an oral medication that controls blood sugar and does not cause weight gain. The drug is often prescribed for overweight and obese subjects, but the effectiveness of the drug is still similar to that of non-obese people. It works by reducing blood sugar by inhibiting gluconeogenesis.
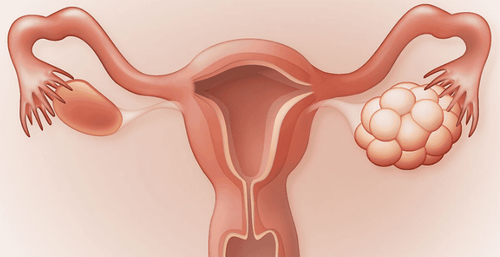
Metformin is indicated in the treatment of non-insulin dependent diabetes mellitus (type 2 diabetes): Used as monotherapy when the hyperglycemia cannot be treated with diet alone. In addition, metformin can be used in combination with a sulfonylurea drug group, and in combination with a strict diet. In fact, metformin or a sulfonylurea alone will not provide adequate blood glucose control.

Thuốc được chỉ định điều trị bệnh lý đái tháo đường
2. Instructions on how to use Biguanide (metformin) antidiabetic drugs
Metformin is usually approved by your doctor in the following doses:
2.1. Metformin Immediate Release (IR) Initiation: 50mg twice daily or 850mg once daily; Increase dose: Gradually increase 500mg weekly or 850mg over 2 weeks; Maintenance dose: 2000mg/day; Maximum dose: 2500mg/day. Note: Biguanide group should be used after breakfast and dinner, swallow whole, do not crush, do not chew.
2.2. Metformin Extended Release (ER) Initiation: 500 - 1000mg once a day; Increase dose: Increase slowly by 500mg per week; Maintenance dose: 2000mg/day; Maximum dose: 2500mg/day. Note: If the extended-release form is used but the desired blood glucose level is not achieved, dose splitting should be considered. If a higher dose level is required, an immediate-release formulation should be used.
>> See more: Groups of drugs to treat diabetes

Dùng thuốc điều trị đái tháo đường cần tuân thủ đúng phác đồ điêu trị của bác sĩ
3. Note when using Biguanide (metformin) in the treatment of diabetes
3.1. Undesirable effects of metformin In the process of using the drug may occur undesirable effects, specifically as follows:
Digestive disorders (common in about 5% - 20% of patients): abdominal pain, cramps, diarrhea, nausea or vomiting, acne, loss of appetite, sometimes a metallic taste in the mouth,... These reactions often appear quite early in the course of drug use. metformin is used to treat diabetes, but it is reversible and tapered if the dose is increased sensibly, slowly, and taken at the end of a meal; Reduced absorption of vitamin B12: in many cases, patients need to be supplemented with this vitamin so that the body does not lack cobalamin leading to anemia, fatigue and emotional disturbances; Skin reactions (rare): urticaria, pruritus and erythema.
3.2. Lactic acidosis (very rare - mortality up to 50%) Patients present with cramps, severe muscle weakness, abdominal or chest pain. This is a state of metabolic acidosis due to the release of H+ from lactic acid.
The cause was diagnosed as the mechanism of metformin inhibiting the gluconeogenesis from various sources, including lactate. Accumulation of metformin can exacerbate other causes, such as renal failure, liver failure, hypoxic conditions, poor blood sugar control,...
Therefore, metformin is contraindicated in these conditions. the following cases:
Renal dysfunction; Congestive heart failure requiring drug treatment; Allergy to metformin; Acute or chronic metabolic acidosis; Decreased liver function ; Women who are pregnant and breastfeeding.

Phụ nữ đang mang thai thuộc nhóm đối tượng chống chỉ định dùng thuốc
People with alcoholism are advised to exercise extreme caution when taking metformin. Metformin is also not an appropriate choice in the treatment of elderly people because this age group is often prone to impaired renal function. Therefore, for elderly patients, serum creatinine should be carefully checked before initiating treatment.
3.3. Drug-Drug Interactions For iodinated contrast agents (potential for nephrotoxicity, increased risk of acidosis): Metformin should be discontinued in case of a need for iodinated contrast agents (about 48 hours before). and post-injection) due to the risk of renal failure and lactic acidosis. Similarly, if surgical anesthesia is required, the patient should temporarily discontinue metformin; Drugs affecting glucose metabolism, increasing the glycemic index, including chlorpromazine, glucocorticoids, high-dose progesterone and drugs with sympathomimetic effects; Due to the low degree of plasma protein binding, metformin usually does not interact strongly with drugs that are strongly bound to plasma proteins (such as salicylates, sulfonamides, probenecid, ..). On the other hand, metformin has the ability to interact indirectly (through a competitive mechanism) with drugs that are eliminated in the renal tubule in the form of cations (including some drugs such as amiloride, morphine, quinidine, ranitidine, trimethoprim, vancomycin, .. .). In fact, these cationic molecules are also eliminated by the renal tubule, thus possibly competing with metformin. This phenomenon causes an increase in the plasma concentration of metformin, thereby increasing the risk of lactic acidosis;

Tham khảo ý kiến bác sĩ, dược sĩ trước khi sử dụng thuốc
Careful supervision is required when metformin is used concomitantly with diuretics, non-steroidal anti-inflammatory drugs (NSAIDs), antihypertensives, insulin, sulphonamides, azole antifungals and medicinal preparations contain alcohol. In addition, dose adjustment of metformin is required depending on the clinical course and laboratory test results (serum creatinine, transaminase,...). All patients using metformin to treat diabetes need to adhere to treatment, perform regular check-ups and follow-up as directed:
Every 3 months: HbA1c test (assess blood glucose level in the last 3 months) most), monitor blood pressure, weight; Annual: Examination of fundus area, blood creatinine test, micro-albuminuria, electrolyte assessment, foot examination, blood lipid monitoring. The treatment of diabetes is a long process and requires perseverance, not only relying on medical treatment with antidiabetic drugs but also in combination with lifestyle changes and dietary adjustments. reasonable.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.