This is an automatically translated article.
Article written by Doctor of Laboratory - Vinmec Danang International General Hospital
Urine test is a method to help you know the signs of dangerous and latent diseases in your body and your health situation. However, not everyone knows how to collect clean and correct urine to do the best test.
III. Method of collecting urine culture samples
1.Urine collection midstream
Midstream urine collection is the most common method. Patients should collect samples in the early morning, this is the best time, the first urine volume of the day will be concentrated, so the concentration of bacteria will be higher than other times later.
Before that, the patient needs to clean the external genitalia. To help protect the urine sample from bacteria residing on the penis or vagina that may interfere with test results.
For men : Wash hands thoroughly pull back the foreskin and clean the tip of the penis thoroughly with clean gauze. For women: Wash your hands and expose the folds of skin around the vagina with one hand, with the other hand, use a clean gauze to clean the area around the vagina and urethra thoroughly from front to back to avoid pull bacteria from the anus to the urethra.

Không nên để máu kinh nguyệt dính trong mẫu nước tiểu tránh lây nhiễm vi khuẩn từ môi trường bên ngoài
Note :
To avoid bacterial infection from the outside environment. Do not touch the edge of the vial to the external genitalia and do not let the line get stools, menstrual blood ... in the urine sample. To avoid the proliferation of bacteria in the urine sample. Rapidly transport the urine sample to the laboratory for technical analysis within one hour. If the urine sample cannot be delivered to the laboratory within an hour, the urine sample should be stored in the refrigerator for a maximum of 4 hours.
2.Urine collection through bladder catheter
The method is often applied to people who are seriously ill, unable to collect urine on their own and have difficulty moving. The medical staff will use a small catheter through the urethra to enter the bladder, allowing urine to flow through the tube into a sterile vial.

Đặt sonde bàng quang cho bệnh nhân
3.Urine collection through suprapubic needle aspiration
This method guarantees the best quality of the collected urine sample. However, it is very complicated, so it is only conducted in special cases with a prescription from a doctor.
4. Several factors may affect the culture results
If the amount of urine is too low, it will affect the test results.
Obtaining a urine culture before a patient is on a diuretic can dilute the urine and also reduce the number of bacteria in the specimen.
Obtaining a urine culture while taking antibiotics or just finishing a course of antibiotics will also affect test results.

Người lấy nước tiểu đang sử dụng thuốc lợi tiểu có thể làm loãng nước tiểu và cũng làm giảm số lượng vi khuẩn trong mẫu bệnh phẩm.
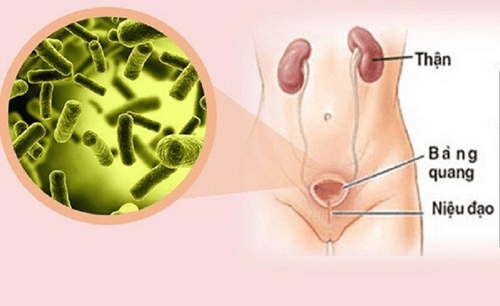
IV . Bacterial causes of urinary tract infections
The cause of infection is also very diverse, but it is mainly caused by bacteria. Especially, upstream urinary tract infections are often caused by Gram-negative bacteria, mainly belonging to the Enterobacteriaceae group such as bacteria: E.coli, Klebsiella, Proteus...
In bacterial etiologies, Gram-negative bacteria are still majority. In 25% of cases, multiple cultures can be isolated at the same time. Common bacterial causes are:
1. Intestinal gram-negative bacteria
Escherichia coli, Proteus spp, Klebsiella spp Enterobacter spp...
2. Non-intestinal gram-negative bacteria
Common causes of hospital-acquired infections are:
Pseudomonas aeruginosa, Pseudomonas spp, Acinetobacter baumannii ...
3. Gram-positive cocci
Enterococcus spp, Staphylococcus sprophyticus, Staphylococcus aureus and Group B Streptococcus ...
4.Other causes
Neisseria gonorrhoeae, Chlamydia trachomatis, Candida albicans and tuberculosis ...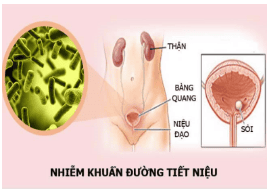
Nhiễm khuẩn đường tiết niệu
V. Multi-antibiotic-resistant enteric gram-negative bacteria cause urinary tract infections
1. Transmission mechanism of antibiotic resistance
Gram-negative bacteria of the enteric family are mainly responsible for urinary tract infections, the main mechanism of antibiotic resistance in this group of bacteria is the production of broad-spectrum beta-lactamases (ESBL), leading to bacterial infection. bacteria resistant to all beta-lactamines.
For the first time in 1983, the production of broad-spectrum beta-lactamases (ESBL) by gram-negative enteric bacteria (Enterobacteriaceae) by plasmide transmission was discovered in Germany and then in the United States. The yeast ESBL was first identified in the Klebsiella pneunomiae strain.
Then through the yeast plasmide ESBL is quickly and easily transmitted to other enteric gram bacteria, especially Escherichia coli. Currently, these two strains of gram-negative bacteria are the two most common ESBL-producing strains, the other strains are rarer.
Due to the above transmission mechanism, the rate of cephalosporinases is very high in intestinal gram-negative bacteria such as E. coli; Klebsiella pneumonia; Enterobacter and Citrobacter. Gene AmpC was identified as related to cephalosporinases. There are more than 20 different types of lactamases belonging to the Amp-C type, so the intestinal gram-negative bacteria are very resistant to the antibiotics of the lactamines group.
2. Causes and consequences of increasing antibiotic resistance in bacteria

Sử dụng thuốc kháng sinh fuoroquinolones làm biến đổi đích tác dụng của kháng sinh và bơm đẩy thuốc ra ngoài làm giảm nồng độ kháng sinh bên trong vi khuẩn
The prevalence of antibiotic-resistant gram-negative bacteria has increased significantly globally due to the overuse of antibiotics especially in the community. A Canadian statistic shows that every year about 25 million antibiotics are prescribed and over 50% of them are prescribed inappropriately, so it is not surprising that the situation of bacterial resistance develops. .
According to many different studies, the rate of inappropriate use of antibiotics accounts for about 40-75%. The useless exposure to antibiotics not only increases the risk of patient toxicity, side effects, drug interactions, superinfection, but also is a major cause of the spread of drug resistance leading to gram-negative bacteria. The intestinal tract produces broad-spectrum beta-lactamases (ESBLs) that are sensitive only to cefepime and to carbapenemes.
Along with resistance to beta-lactamines, resistance to fluoroquinolones of intestinal gram-negative bacteria is growing.
The main reason is the increased use of antibiotic fuoroquinolones in the community for the treatment of pneumonia, urinary tract infections, skin and soft tissue infections. Mechanism of resistance to fluoroquinolones antibiotics in two ways: changing the target of the antibiotic and pumping the drug out to reduce the concentration of antibiotics inside bacteria.
The increasing antibiotic resistance of bacteria is one of the dilemmas facing clinicians and microbiologists today. Measures to control and prevent the spread of Enterobacteriaceae producing broad-spectrum β-lactamase or plasmid-mediated AmpC β-lactamase in hospitals and the community are urgently needed, especially the use of drugs. Safe and reasonable antibiotics are very important.
BECAUSE. Prevention of urinary tract infections

Nên ăn nhiều loại trái cây như chanh, bưởi,cam thường xuyên giúp bệnh nhiễm khuẩn đường tiết niệu
To prevent urinary tract infections and especially to avoid the recurrence of urinary tract infections after treatment, patients need to have the following good habits:
Drink plenty of water (2 liters/day) to clean the bladder, eliminate harmful components, avoid the proliferation of pathogens. Should eat a variety of fruits such as oranges, lemons, grapefruit regularly. These fruits make urine acidic, making it difficult for bacteria to grow in an acidic environment. When urinating, don't hold back but go immediately, don't even wait for the feeling of needing to urinate, but wait for 2 to 3 hours to urinate by yourself. The more stagnant urine is, the more likely pathogens are to develop. After each intercourse, women should urinate immediately and clean the vaginal area to remove bacteria that are introduced into the urethra and bladder. The private area must be cleaned once a day, when washing should be done from front to back, to avoid bringing bacteria available in the vulva and anus into the urinary tract. During the menstrual cycle, women have to change the dressing often even though there is little bleeding. Another important thing that patients need to pay attention to is to choose a reliable, quality and qualified medical facility to perform. Vinmec International General Hospital is one of the hospitals that not only ensures professional quality with a team of leading medical professionals, a system of modern equipment and technology. The hospital provides comprehensive and professional medical examination, consultation and treatment services, with a civilized, polite, safe and sterile medical examination and treatment space. Customers when choosing to perform tests here can be completely assured of the accuracy of test results.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.