Dilated cardiomyopathy (DCM) is a fairly common cardiovascular disease that frequently leads to heart failure. But how dangerous is dilated cardiomyopathy, and how can it be diagnosed and treated to limit complications and improve survival rates?
1. What is Dilated Cardiomyopathy?
1.1 Definition
Dilated cardiomyopathy (DCM) is a condition characterized by the enlargement and dilation of one or both ventricles, with normal wall thickness of the left ventricle, accompanied by impaired contraction function. This is defined by a left ventricular ejection fraction (LVEF) below 40%.
Patients with DCM experience systolic dysfunction and may or may not display overt heart failure symptoms. DCM can be classified into two categories: primary (idiopathic) or secondary. Primary dilated cardiomyopathy is considered idiopathic, and the diagnosis is made after ruling out secondary causes.
1.2 Epidemiology
The prevalence of DCM is estimated to affect 1 in 2,500 people.
Genetic factors account for approximately 35% of cases.
It often occurs in adults between 20-60 years old, though children can also be affected.
DCM is more common in men than women.
Certain genetic variants are found more frequently in African Americans than in Caucasians.
2. Causes and Risk Factors of Dilated Cardiomyopathy
Family history of DCM, heart failure, or sudden cardiac arrest.
Autoimmune diseases such as systemic lupus erythematosus or rheumatoid arthritis.
Neuromuscular disorders, such as muscular dystrophy.
Infections
Complications from late pregnancy (third trimester – 28 to 40 weeks).
Diabetes mellitus.
Hemochromatosis (iron overload disorder).
Arrhythmias, such as atrial fibrillation.
Hypertension.
Obesity.
Valve diseases, such as mitral regurgitation or aortic regurgitation.
Alcohol abuse.
Exposure to toxins like lead, mercury, or cobalt.
Certain chemotherapy drugs.
Illicit drug use, such as amphetamines or cocaine.
3. Diagnosis
3.1 Clinical Symptoms
Patients with DCM may exhibit a range of symptoms depending on the severity of the condition, including:
Fatigue.
Shortness of breath, either during physical activity or at rest.
Reduced exercise tolerance.
Swelling of the legs, ankles, feet, or abdomen, often accompanied by weight gain and abdominal distension.
Prominent neck veins (jugular vein distension).
Dizziness or fainting spells.
Chest pain or discomfort.
Rapid or irregular heartbeats (palpitations).
3.2 Diagnostic Tests
Chest X-Ray: may show an enlarged heart silhouette or pulmonary edema.
Electrocardiogram (ECG): could reveal sinus tachycardia, left bundle branch block, or ST and T wave abnormalities.
Echocardiogram: the primary imaging tool used to assess left ventricular dilation and impaired systolic/diastolic function. May also show mitral or tricuspid regurgitation.
B-Type Natriuretic Peptide (BNP): often elevated in heart failure; useful for diagnosis and prognosis.
Coronary Angiography: typically reveals normal coronary arteries in DCM patients.
Endomyocardial Biopsy: rarely performed, unless necessary to exclude specific myocardial disorders like myocarditis, amyloidosis, sarcoidosis, or hemochromatosis.
4. Can Dilated Cardiomyopathy Be Treated?
Dilated cardiomyopathy may be treated using a variety of ways, which have yielded several favorable outcomes. Effective treatment strategies focus on improving heart function, alleviating symptoms, and preventing complications. Treatment is similar to that of heart failure and includes:
Diuretics: Loop and thiazide diuretics help alleviate fluid overload in symptomatic patients.
ACE Inhibitors: Recommended for patients with reduced ejection fraction to improve heart function.
Angiotensin receptor blockers (ARBs) may be used as alternatives.
Digoxin: Beneficial for patients with persistent symptoms despite diuretics and ACE inhibitors or those with atrial fibrillation.
Beta-Blockers: Proven to reduce mortality and complications in all DCM patients.
Spironolactone: Demonstrated to lower mortality rates in patients with severe symptoms.
Nitrates: Helpful for diastolic dysfunction and pulmonary congestion.
Anticoagulants: Indicated for patients with atrial fibrillation, artificial heart valves, or intracardiac thrombi.
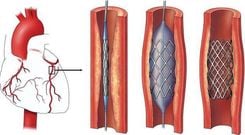
Implantable Cardioverter Defibrillators (ICDs): Reduce the risk of sudden cardiac death in high-risk patients.
Surgical Interventions: Mitral valve repair or replacement can alleviate symptoms in cases of severe mitral regurgitation.
Catheter ablation may be useful for patients with recurrent ventricular tachycardias.
Advanced Therapies: Some patients, especially younger individuals, medical therapies may not be effective, requiring left ventricular assist devices (LVADs) or heart transplantation.
Stem Cell Therapy has shown promise in improving left ventricular ejection fraction (LVEF) and reducing left ventricular end-systolic volume and left ventricular end-diastolic dimensions in patients with dilated cardiomyopathy. However, further research is needed to fully understand the effects and potential applications of stem cell therapy in this patient group.
5. Is Dilated Cardiomyopathy Dangerous?
5.1 Complications of DCM
Dilated cardiomyopathy can lead to serious complications, including:
Heart Failure: The most severe consequence, potentially life-threatening if untreated.
Valve Regurgitation: DCM may impair valve function, causing blood to leak backward, particularly through the mitral valve.
Arrhythmias: Enlargement and altered heart shape increase the likelihood of abnormal heart rhythms.
Sudden Cardiac Arrest: Malignant arrhythmias can cause the heart to stop suddenly.
Pulmonary hypertension, diastolic dysfunction.
Thromboembolism: Blood clots forming in the left ventricle can travel to other organs, causing strokes, heart attacks and other complications. Heart rhythm disorders such as atrial fibrillation can also cause blood clots.
5.2 Prognosis
The prognosis of DCM is closely related to the severity of initial symptoms. Additionally, factors such as fluid and sodium restriction, medication adherence, and regular exercise can significantly influence outcomes.
The one-year survival rate for patients with DCM is approximately 80%, decreasing by about 10% each subsequent year. The five-year survival rate is roughly 50%. Complications such as mitral valve regurgitation or diastolic dysfunction are associated with a poorer prognosis.
Sudden cardiac death accounts for 40-50% of fatalities, often due to malignant arrhythmias or thromboembolic events.
Congenital cardiomyopathy is also linked to higher rates of morbidity and mortality.
Patients with DCM should be educated on preventive measures and cardiac rehabilitation. This approach has been shown to reduce all-cause mortality by 20-30% within five years, alongside improving symptoms and quality of life.
Research on patients treated with heart transplantation indicates survival rates of 91% after one year, 80% after five years, and 50% after 20 years.
Dilated cardiomyopathy is a serious cardiovascular condition with potentially life-threatening complications. Regular health check-ups and consultations with cardiology specialists are critical for early diagnosis and intervention. With proper treatment, patients can manage their symptoms and improve their quality of life.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.