This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalThe diagnosis of eosinophilic gastroenteritis is confirmed by biopsy or collection of eosinophilic ascites in the absence of other pathogens, including intestinal parasites. Eosinophilic esophagitis should also be differentially diagnosed and discussed.
1. Eosinophilic gastroenteritis
Eosinophilic gastroenteritis (English used from Eosinophilic gastroenteritis_EG) is a disease in the following group of diseases: eosinophilic esophagitis (eosinophilic esophagitis), gastritis, enteritis, colitis eosinophil gastritis, enteritis, and colitisThis is a major histopathologic diagnosis with elevated eosinophil count (BCAT) on biopsies of the gastrointestinal mucosa. and rule out causes of local elevation of BCAT. However, the criteria for histopathology to date have not been agreed, so the role of the pathologist in conjunction with the clinician is very important. The diagnosis of EG is confirmed by biopsy or collection of eosinophilic ascites in the absence of other pathogens, including intestinal parasites. Eosinophilic esophagitis should also be differentially diagnosed and discussed.
2. Under the microscope, what is the nature of these images?
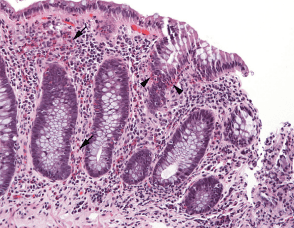
Confirmation of the diagnosis of eosinophilic gastroenteritis must be based on histopathological findings of biopsies taken from the stomach, small intestine (usually duodenum), colon, or rectum. Among the segments of the gastrointestinal tract, the cecum and the appendix are the sites with the highest BCAT counts (up to 30 cells/microfield).Stomach and colon have lower BCAT counts, so the agreed criteria for the diagnosis of eosinophilic gastroenteritis in most studies is when the BCAT count is above 20 cells/microfield. The distribution of BCAT is characterized by regional characteristics, so multiple biopsies including normal mucosal areas help confirm the diagnosis. Using immunohistochemical staining methods also helps determine the deposition of substances released from extracellularly deposited BCAT particles such as MBP, ЕСР. . In the case of myosinophilic or serosa eosinophilic gastroenteritis, it may be necessary to combine with laparoscopy or capsule endoscopy to obtain specimens to confirm the diagnosis.
2.1 Eosinophilic gastritis In contrast to the esophagus, eosinophils are normally present in the gastric mucosa, but in lower concentrations in the small and large intestine. Criteria for the histological diagnosis of eosinophilic gastritis include 30 eosinophils/field in at least 5 fields and 70 eosinophils/field in at least 3 fields. .
Common features of biopsies of eosinophilic gastritis are enlarged stromal eosinophilic plates, excess in eosinophil epithelium, cholecystitis/eosinophilic abscess, and eosinophils in the mucosal muscle and submucosa. Mast cells and FOXP3 factor lymphocytes were more abundant in eosinophilic gastritis biopsies than in controls.
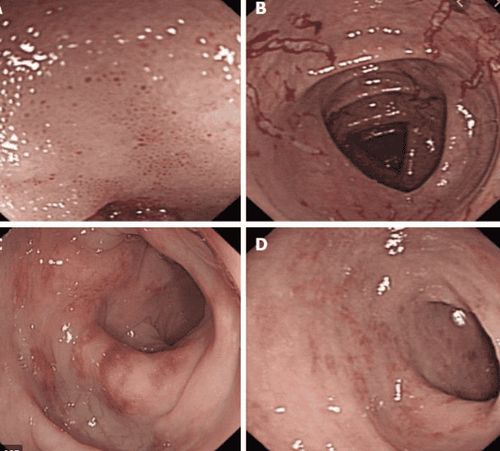
Clinical features of eosinophilic gastritis include epigastric pain, peripheral blood eosinophilia, anemia, and hypoalbuminemia. Endoscopic abnormalities include nodular mucosa, congestion, and ulceration/erosion, but mucosa may be normal.
Eosinophilic gastritis may occur singly or may be associated with excess eosinophil infiltration in the rest of the gastrointestinal tract, especially the esophagus, simultaneously or sequentially. Antigen successfully relieves symptoms and tissue eosinophilia in some pediatric patients with eosinophilic gastritis.
.
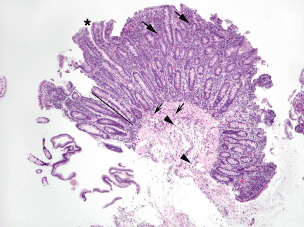
2.3 Eosinophilic colitis Eosinophils are commonly found in the lining of the colon and most commonly in the right colon of both children and adults. Therefore, using a single cut-off value to define eosinophilia is less accurate and potentially misleading than applying appropriate threshold values for each colon site ( right, transverse, left, rectal) were appropriately marked and the colonic mucosa was sent separately for biopsy.
Excess eosinophils can be considered as a multiple of eosinophil peaks/field in a normal biopsy, consisting of 2 × 50 eosinophils/field or 100 eosinophils/ cecum and ascending colon, 2 × 42 eosinophils/field or 84 eosinophils/field in transverse and descending colons, and 2 × 32 eosinophils/field or 64 eosinophils/field in the rectal mucosa. Histological features of colon biopsies showed increased eosinophil density in the epithelium and eosinophils in the muscular mucosa and submucosa.
The prevalence of eosinophilic colitis is difficult to determine, in part, because there are no clinical or pathological diagnostic guidelines.
However, a reasonable approach is that eosinophilic colitis should be a clinical diagnosis, similar to eosinophilic esophagitis, which requires both symptoms to suggest Refers to colonic dysfunction and colon biopsy showing eosinophilia. Colon biopsy showed a greater than normal density of eosinophils. Most of those patients had symptoms, mainly diarrhea and abdominal pain, but about a third were asymptomatic. Endoscopic abnormalities have been reported including hemorrhage, mucosal loss, white lesions, pale granular mucosa, and aphthous ulcers. Several studies have documented that excess eosinophils can be found in mucosal biopsies from patients with IBD.
Neonatal allergic colitis has been diagnosed if > 20 eosinophils/field are found in rectal biopsy, possibly in patchy distribution, resolve clinical follow-up eliminating the offending antigen, usually cow's milk, from the diet of the affected infant. Since this condition is easily, and seemingly permanent, treated by withdrawing a substance from the diet, classification as an esinophilic gastroenteritis is considered inappropriate by some experts.
3. Differential diagnosis with increased eosinophil density
The differential diagnosis of increased eosinophil density in the colonic mucosa is broader than discussed above, and includes parasitic infection, eosinophilic syndrome, etc. The diagnosis is made only after all known causes for colonic eosinophilia have been ruled out.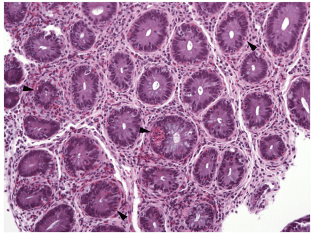
4. Post-treatment follow-up based on histopathological images
During treatment, monitoring response based on which criteria is still controversial. To date in most studies, response to treatment has been primarily based on improvement in clinical symptoms and reduction in BCAT counts. However, it still needs to be combined with changes in endoscopic and histopathological images. According to the 2013 American Gastroenterological Society recommendations, histopathological complete response was defined as a >90% reduction in BCAT counts. Most studies use the maximum number of BCAT counts, some use the mean. In addition, it is necessary to pay attention to other characteristics related to inflammatory tissue damage such as basal proliferation, subepithelial fibrosis... The development of severity grading scales on endoscopy and tissue disease. The study is expected to provide effective tools for monitoring response after treatment. Many aspects of the diagnosis of eosinophilic gastroenteritis, the pathogenesis, therapy, etc., are still to be determined. Recently, the Foundation for Eosinophilic Gastroenterology (CEGIR) has received much help to facilitate studies of these rare diseases. These studies hope to yield insights Basic and clinical science knowledge will lead to and effective therapies.Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit examination and treatment of eosinophilic gastroenteritis at the Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
ReferencesA Lowichik 1, A G Weinberg. A quantitative evaluation of mucosal eosinophils in the pediatric gastrointestinal tract. Mod Pathol. 1996 Feb; 9(2):110-4. Kinoshita Y, Ishimura N, Oshima N et al (2015). Systematic review: Eosinophilic esophagitis in Asian countries. World J Gastroenterol, 21 (27): 8433-40. SEE MORE
Mononucleosis: What you need to know Common dysfunctions in the esophagus and stomach Eosinophils: What you need to know