Gestational diabetes is a condition of impaired glucose metabolism that occurs during pregnancy. This condition can cause significant complications for both the mother and the baby. So, can you have a natural birth with gestational diabetes, or do you need a cesarean section?
1. What is Gestational Diabetes?
Gestational diabetes is a condition of impaired blood sugar levels that occurs during pregnancy. After the mother gives birth, the condition usually resolves. However, gestational diabetes is likely to recur in a second pregnancy if the mother had it during her first pregnancy.
Gestational diabetes is similar to regular diabetes. Most pregnant women with gestational diabetes often show few clear symptoms. Some cases are noticed through frequent urination and constant thirst...
Gestational diabetes is like regular diabetes. Most pregnant women with gestational diabetes often have few clear symptoms. Only a few people notice it through frequent urination, constant thirst... Eating a lot of sweets, consuming fatty foods, cravings, high blood pressure, and lack of exercise are the main causes of the disease.

Currently, the prevalence of gestational diabetes mellitus (GDM) is increasing and shows a rising trend. To date, the pathogenesis of GDM remains unclear. The condition has been associated with cellular insulin resistance, obesity, GDM itself, insulin receptor dysfunction, glucose transport and insulin activity disorders, pancreatic islet dysfunction, autoimmune mechanisms, genetic factors, fetal factors, and inflammatory factors. Among these, cellular insulin resistance is considered the most common mechanism underlying GDM, as nine pathogenic mechanisms of gestational diabetes mellitus have been identified.
Due to the ineffective action of insulin and high insulin resistance, gestational diabetes occurs. The insulin levels in the blood of those with GDM may be high, but the body's cells decrease or do not respond to the effects of insulin.
The appearance and increase of pregnancy hormones lead to these changes. This condition is often not apparent in the early stages of pregnancy. GDM in the second half of pregnancy is likely to occur if there is a decrease in insulin response to changes in blood glucose levels, indicating a decline in pancreatic cell function—the organ that produces insulin.
2. Who is at Risk for Gestational Diabetes?
One of the most common complications during pregnancy is gestational diabetes, affecting 1 in 10 pregnant women and more frequently occurring in those who are obese. By minimizing risk factors, you can manage this condition.
Some factors that increase the risk of gestational diabetes include:
- Women over 25 years old
- Family history of diabetes
- Obesity (BMI >30 increases the risk of gestational diabetes by 3 times compared to those with a BMI < 20)
- Southeast Asians have a 5 times higher rate of diabetes
- History of abnormal glucose tolerance or impaired fasting glucose tolerance
- Previous history of gestational diabetes
- History of giving birth to a baby over 4kg
- Multiple miscarriages, stillbirths, especially in the last trimester, congenital anomalies, polyhydramnios, etc.
- Previous pregnancy with blood pressure disorders, chronic hypertension, or kidney disease

3. Is Gestational Diabetes Dangerous?
Gestational diabetes can have severe consequences for both the mother and the newborn, increasing morbidity and mortality rates.
For the mother, the risk of complications such as metabolic disorders, infections, kidney damage, eye damage, and coronary artery damage increases due to gestational diabetes. Obstetric complications that may occur include hypertension during pregnancy, preeclampsia, difficult labor, birth trauma, postpartum hemorrhage, increased cesarean section rates due to large babies, and increased infection rates.
In the long term, there is a risk of developing type 2 diabetes later (30-50% develop type 2 diabetes within 5-10 years). Obesity and excessive weight gain are also concerns.
There is also a risk of gestational diabetes in subsequent pregnancies (30-69% in subsequent pregnancies).
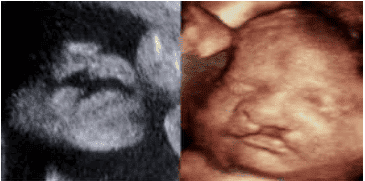
For the fetus, gestational diabetes significantly affects fetal development. Gestational diabetes impacts two stages of fetal development:
The first trimester of pregnancy: Gestational diabetes affects the development of the embryo and fetus, leading to spontaneous miscarriage, stillbirth, and congenital anomalies with a rate of 8-13%, which is 2-4 times higher than in those without gestational diabetes. Common anomalies include damage to the nervous system, heart, large blood vessels, skeletal system, kidneys, and urinary system.
The third trimester of pregnancy:
- Increased perinatal mortality rate (20-30%), especially post-delivery due to hypoglycemia and hypocalcemia. The mother's chronic hyperglycemia leads to increased glucose utilization by the fetus, causing fetal hypoxia and acidosis, which directly affects stillbirth, potentially leading to fetal death within the last 3-6 weeks of pregnancy.
- Increased rates of respiratory distress syndrome, hyaline membrane disease, and lung collapse due to impaired lung development.
- Excessive fetal growth, macrosomia.
- Risk of preterm birth due to acute and chronic polyhydramnios.
- Fetal growth restriction.
- Oligohydramnios.
- Macrosomia, difficult labor causing trauma.
4. Should You Have a Natural Birth or a Cesarean Section with Gestational Diabetes?
If the mother can control her blood sugar levels, the pregnancy can proceed normally without affecting the delivery. Whether to opt for a cesarean section or vaginal delivery depends on many obstetric reasons that are difficult to predict during pregnancy. Predictions can be more accurate closer to delivery or labor.

5. What Should You Do If You Have Gestational Diabetes?
Pregnant women with gestational diabetes should take the following measures:
Maintain a healthy and reasonable diet:
- The body does not produce insulin to convert sugar into energy, causing it to accumulate in the blood.
- Pregnant women should avoid foods high in sugar. Minimize fats and animal fats, and avoid fried foods high in cholesterol. Before consuming, check the nutritional content on the packaging of packaged and canned foods.
Exercise regularly and consistently:
- Regular exercise helps move blood sugar to other cells, reducing its presence in the blood.
- Pregnant women should exercise gently, keeping their heart rate below 140 beats per minute. With 30 minutes of exercise each day, the body can easily absorb glucose, combat diabetes, and alleviate symptoms like back pain and cramps.

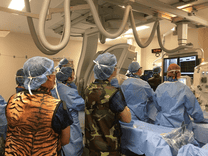
Regular Check-ups:
- Pregnant women should visit their doctor for examinations and prescription advice when diagnosed with gestational diabetes. They must regularly check their blood sugar levels to monitor changes promptly, proactively prevent, and manage the condition effectively during treatment.
- The doctor will adjust the insulin dosage based on the mother's condition during the examination. Some medications are not suitable for pregnant women and can lead to miscarriage and other unfortunate consequences, so pregnant women should never self-medicate.