This is an automatically translated article.
Post of MSc. Dr. Le Thi Thanh Huong - Emergency Resuscitation Doctor - Emergency Resuscitation Department - Vinmec Central Park International General Hospital
People with gastroesophageal reflux disease (GERD), also known as "acid reflux" occurs when gastric juices back up into the esophagus and/or mouth. Occasional reflux is normal and can occur in otherwise healthy infants, children, and adults, most often after eating a meal. Most reflux episodes are brief and do not cause uncomfortable symptoms or complications. In contrast, people with GERD experience uncomfortable symptoms or damage to the esophagus as a result of acid reflux. Symptoms of GERD can include heartburn, regurgitation, and difficulty swallowing or pain when swallowing.
1. What is gastroesophageal reflux disease?
Gastroesophageal reflux disease (GERD) is a condition that occurs when the digestive juices of the stomach regularly back up into the esophagus (the tube that carries food from the mouth to the stomach). Because this fluid is acidic, it can irritate and inflame the lining of your esophagus.Most people can manage the discomfort of GERD with lifestyle changes or self-medication (over-the-counter drugs) from the pharmacy to take. But some more severe cases may need to see a doctor to be prescribed stronger drugs or even surgery to relieve symptoms caused by it
2. Causes of Gastroesophageal Reflux Disease (GERD)
Is caused by frequent reflux of stomach acid or bile into the esophagus. When you swallow, the lower esophageal sphincter (the ring of muscle that surrounds the bottom of the esophagus) relaxes to allow food and liquid to pass down to the stomach, where it then closes. However, if this muscle relaxes abnormally or becomes flaccid, stomach acid can back up into the esophagus, causing you to experience frequent heartburn, affecting your daily life.
Constant acid reflux can cause inflammation in the lining of your esophagus. Over time, inflammation wears away this layer, causing complications such as bleeding, narrowing of the esophagus, or Barrett's esophagus (precancerous lesions).
Risk factors: the following conditions can increase your chances of developing acid reflux:
Obesity The upper part of the stomach that runs up to the chest (diaphragmatic hernia) Pregnancy Smoking Dry mouth Asthma Diabetes Prolonged gastric emptying Disorders of the connective tissue such as scleroderma

3. Signs, symptoms and symptoms of gastroesophageal reflux disease
To recognize GERD is relatively difficult, because the symptoms of the disease are often confused with other diseases. However, when you find yourself with many signs that correspond to the following symptoms, you should be alert because you may have GERD:
Common signs and symptoms of GERD include: include:
slightly : happens often and even when hungry or not eating. Heartburn: Burning from the stomach or lower chest area, spreading up the neck, sometimes spreading to the lower throat and ears. Along with that is the sour taste in the mouth. Heartburn: Acidic food or liquid from the stomach is pushed up the throat usually after eating, which can be worse at night. Vomiting and nausea: appear when eating too full, lying down right after eating, do not raise your head when sleeping. Feeling of heat in the chest, tightness in the chest Lots of saliva, difficulty swallowing, feeling stuck in the throat...
If you have acid reflux at night, you may also experience:
Chronic cough Laryngitis New or worsening asthma Disrupted sleep When to see a doctor?
Go to the hospital immediately if you feel chest pain, especially if you have other symptoms such as: pain spreading to the shoulder, arm or chin, shortness of breath, dizziness ... because in addition to reflux disease Gastroesophageal reflux can be a symptom of a heart attack.
See a doctor if:
- Symptoms get worse or occur more often.
- You have bought yourself and taken stomach medicine more than 2 times/week, but still no improvement.
4. Harms and complications of gastroesophageal reflux disease
Due to the lack of understanding of the severity of reflux esophagitis, many people have shown indifference to this disease. In fact, reflux esophagitis causes many dangerous complications, such as esophageal stricture, esophageal ulceration and, in the worst case, esophageal cancer. Therefore, you should not be subjective when you find yourself having symptoms of GERD.
Over time, chronic esophagitis can lead to the following complications:
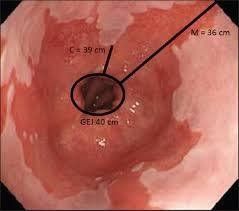
Esophageal stricture: damage to the cells in the lower sphincter of the esophagus caused by prolonged exposure to stomach acid, which forms tissues scar. This scar tissue narrows the esophagus, making it difficult to swallow. Esophageal ulcers: Stomach acid can severely erode tissues in the esophagus, creating ulcers. This esophageal ulcer can bleed, make it painful and difficult to swallow. Precancerous changes in the esophagus (Barrett's esophagus): In Barrett's esophagus, changes in the tissue lining the lower esophagus are associated with an increased risk of esophageal cancer. Although the chances of developing cancer are very low, your doctor will still do an esophagoscopy to look for early warning signs of esophageal cancer.
5. Treatment of gastroesophageal reflux disease
Prepare before you see a doctor
If you think you have acid reflux, you should see a specialist. Because often the time for medical examination is very short and you have many questions to ask, you need to be well prepared.
Here's some information to help you prepare before you go to the doctor:
When you make your appointment, ask what you need to avoid (for example, do you need to fast? do you need to stop taking medications? ?...) or do you need to prepare anything else before going to the doctor? Record all of the symptoms you are experiencing, including those that may seem unrelated to the reason for your visit. Jot down key facts about yourself, including stressors or recent life changes. Make a list of all medications, vitamins or supplements you are taking. Consider bringing a friend or family member. Sometimes it can be difficult to absorb all the information provided during a medical visit. Having an extra person with you will help you remember things that you forget or miss. Write down the questions you need to ask your doctor. Diagnosis
To diagnose acid reflux is based on:
Your symptoms: your doctor can diagnose you with acid reflux based on frequent heartburn attacks and other symptoms. Esophageal Acid Monitor Test: Measure esophageal pH with a probe that uses an instrument to measure acidity over 24 hours. The device determines what time of day and for how long stomach acid flows up into the esophagus. One type of this device is a thin, flexible tube that is threaded from the nose down the esophagus. This tube is connected to a small computer worn around the waist or to a shoulder strap. Another model is a small clamp that is placed in the esophagus during esophagogastroduodenoscopy, the transducer transmits information to a small computer worn on the body. After about two days, the probe falls out in the stool. Your doctor may ask you to stop taking your acid reflux medication for this test. If you have acid reflux and you're going to have surgery, you may need additional tests: Upper gastrointestinal X-ray: this is also called a barium X-ray. In this test you must drink a white solution to coat the inner layer of the digestive tract. You will then have an X-ray of the upper part of your digestive tract. This white coating helps the doctor see the shadow of the esophagus, stomach, and upper part of the small intestine (duodenum). Esophagoscopy (using a flexible, flexible tube to look at the esophagus): esophagogastroduodenoscopy is a way to visually examine the inside of your esophagus and stomach. During an endoscopy, your doctor threads a thin, soft, flexible tube with a light and a camera down your throat. Your doctor may also use an esophagoscope to take a biopsy sample for further testing. Endoscopy is valuable in finding complications of diseases such as Barrett's esophagus. Esophageal motility test (esophageal manometry): This test measures movement and pressure in the esophagus. This test involves placing a catheter from your nose down your esophagus. Treatment
Treatment for heartburn and other symptoms of acid reflux usually begins with over-the-counter medications used to control acid. If you don't feel better after a few weeks of taking the medicine, your doctor may change your treatment, including medication and surgery.
Initial treatment for heartburn management
The following over-the-counter medicines can help control heartburn, including:
Acid neutralizers: relieve symptoms quickly but they do not heal the part. The esophagus becomes inflamed due to stomach acid. Taking too much of this medicine can cause side effects such as diarrhea or constipation. Acid-reducing agents: These drugs are not as fast-acting as antacids, but provide significant symptom relief and can reduce acid production for up to 12 hours. Medicines that block acid production and heal the esophagus: These drugs are stronger than the above and help the damaged esophagus heal. Contact your doctor if you need to take these medications for 2 to 3 weeks or if your symptoms do not improve.
Prescribed medications
When visiting a doctor, your doctor may prescribe the following:
H2 receptor blockers (Anti H2) Proton pump inhibitors (PPIs) Generally these are absorbed and have Works well, but long-term use can increase the risk of bone fractures and vitamin B12 deficiency.
Lower esophageal sphincter: This drug can reduce the frequency of relaxation of the lower esophageal sphincter, thereby reducing gastroesophageal reflux. This drug is less effective than proton pump blockers, but it can be used in severe cases. The drug has significant side effects, the most common being fatigue or confusion. Gastroesophageal reflux disease drugs are sometimes combined to increase the effectiveness of treatment.
Surgery and other treatments are used if medication fails
Often GERD can be controlled with medication. In cases where medication doesn't work or you want to avoid its use for a long time, your doctor may recommend more invasive treatments such as:
Surgery to strengthen the esophageal sphincter Lower: This surgery tightens the lower esophageal sphincter to prevent reflux by tying the top of the stomach around the end of the esophagus. This surgery is usually done laparoscopically, in which the doctor makes three or four small holes in the abdomen and inserts surgical instruments such as a flexible tube containing a tiny camera through the opening in the abdomen. Surgery to tighten the lower esophageal sphincter (Linx): Linx is a ring of tiny titanium magnets wrapped around the junction between the esophagus and stomach. The attraction created by the magnets between these particles is strong enough to keep food from backing up into the esophagus through the junction and loose enough for food to pass from the esophagus to the stomach. This Linx ring can be attached to the body with minimally invasive surgeries. The device has been approved by the Food and Drug Administration (FDA), and early studies appear to be promising. Note that: Currently, the treatment of reflux esophagitis is not too difficult, so you just need to contact a specialist doctor and follow the treatment regimen given by the doctor.

6. Prevention of gastroesophageal reflux disease
To prevent reflux esophagitis, we need to pay attention to our diet as well as keep our spirits up. Avoid being overweight or obese. Lifestyle changes can help reduce the frequency of heartburn.
Consider doing the following:
Maintain a normal weight: excess weight puts pressure on the abdomen, pushing the stomach up and causing stomach acid to back up into the esophagus. If your weight is in the normal range, work out to stay at that weight. If you are overweight or obese, work out to lose weight slowly – lose no more than 0.5-1kg/week. Consult your doctor for appropriate weight loss advice. Avoid wearing clothes that are too tight: clothing that is too tight around the waist will increase abdominal pressure and exert pressure on the lower esophageal sphincter. Avoid foods and drinks that cause heartburn: each person has a different type of trigger food and drink. Foods and drinks such as fried, greasy, ketchup, alcohol, chocolate, mint, garlic, onions, and coffee can make heartburn symptoms worse. Avoid foods that you know will give you heartburn. Eat small meals: avoid eating too much in one meal by eating many meals throughout the day. Do not lie down immediately after eating: wait at least 3 hours after eating before lying down or going to bed. Elevate the head of your bed: if you have frequent heartburn at night or just starting to sleep, let gravity help. Place a piece of wood or a few blocks of cement - at the foot of the bed so that the head of the bed is 15 - 23 cm high. If you can't raise the head of the bed, you can insert a bed wedge between the mattress and the bed to raise your upper half from the waist up. Bed wedges can be found at drugstores and medical supply stores. Elevating the head with extra cleats doesn't work. Don't smoke: Smoking reduces the ability of the lower esophageal sphincter to function properly.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.