This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalEndoscopic retrograde cholangiopancreatography allows visualization, feeling the firmness (hard-soft) of the great duodenal papilla, assessing the function of the sphincter of Oddi by sphincter of Oddi manometry and radiographic imaging of the muscles. Tubular organs can be affected by papillary stenosis.
1. Reasons for not being able to insert a catheter into the great duodenal papilla during endoscopic retrograde cholangiopancreatography
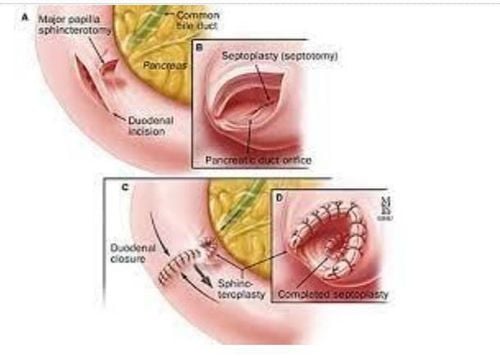
In the majority of patients with papillary stenosis, the papillae are normal when viewed macroscopically on endoscopic examination. Failure to insert a catheter into the major papilla, i.e. sphincter of Oddi stenosis according to Zimmon, Falkenstein and Clemett 1978.
Failure to insert a catheter into the major papilla, the authors found, could be due to:
Obstruction due to any cause (u, gravel, poor technique). Dysfunction of the muscle of Oddi can make it difficult to insert a large duodenal papillary catheter. Although papillary stenosis does not have a specific radiographic image on NTDs (Zimmon, Falkenstein and Clemett 1978; LoGuidice 1979), however, some abnormalities can be noted on radiographs such as:
Dilatation of the bile duct. Slow drainage of contrast material in the bile duct. Abnormal pancreatic radiographs (Gregg 1978, Raskin 1978). The most common is the narrowing of the common bile duct near the great duodenal papilla.
2. Definition of slow drainage of contrast in the biliary system
The bile duct is still visible on radiographs after 45 minutes of retrograde pumping and the absence of a gallbladder. However, the value of this method has not been well studied. In practice, this method is rarely used.
Compensatory dilation of the extrahepatic bile duct usually does not occur after cholecystectomy (Graham 1980, Mueller 1981) if the diameter of the extrahepatic bile duct was normal before cholecystectomy. If the bile duct was dilated before surgery but still dilated after surgery, only a few cases of diameter returned to normal.
The explanation mechanism is as follows:
Incompleteness of the bile duct elastic fibers due to long-term obstruction. Small stones are difficult to detect. If after cholecystectomy, the extrahepatic bile duct increases in diameter, there is obstruction. If the patient is asymptomatic, the progression is very slow, intermittent, possibly due to stones or disorders of the sphincter of Oddi. Bile duct dilatation is a reliable indicator of obstruction at the large duodenal papilla, especially as the diameter increases, but there are cases of papillary stenosis but the diameter of the bile duct is not dilated, according to Raskin (1978) in 83% of patients. Patients with papillary stenosis but normal bile duct diameter.

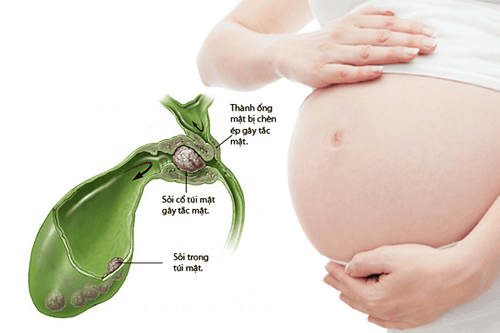
3. Measuring sphincter of Oddi pressure through endoscopic cholangiopancreatography
The typical results of sphincter pressure measurement by normal infusion method are that the common hepatic duct pressure is 10 mmHg greater than the duodenal pressure and the baseline pressure of the sphincter of Oddi is 10-17 mmHg greater than the duodenal pressure. In addition to the background pressure, there is also the cyclical pressure. The normal value of this cyclic pressure is highly variable in frequency ranging from 2.6 to 7.5 mmHg: Cendes 1979, Geenen 1980, Carr-Locke 1981, Touli 1982 and De Masi 1984. Cyclic wave-mean peak amplitude can determine the direction of the cyclic wave of the sphincter of Oddi if a 3-inlet catheter is used.
4. The sphincter of Oddi works independently of the duodenal muscle
The important thing is that the sphincter of Oddi works independently of the duodenal muscle. Embryologically, the sphincter of Oddi develops separately from the duodenal muscle, which binds only towards the end of pregnancy (Boyden 1937, Schwegler 1937). Several animal studies have shown that sphincter of Oddi function is distinct from duodenal function (Hauge and Mark 1965, Hedner and Rorsman 1969, Ono 1970, La Morte 1980). Evidence from simultaneous electromyography of the sphincter of Oddi and duodenum shows that the mechanical activity of the sphincter of Oddi is not directly related to the duodenum (Ishioka 1959, Ono 1970).
Methods to determine if the catheter is already in the bile duct include:
Bile aspiration (Staritz, Poralla and Ewe 1985); Contrast injection; Insert the catheter after swimming upstream, and at the same time aspirate contrast; The catheter follows the path of the bile duct. Many drugs are used routinely in endoscopy but without Diazepam (Webel 1975), stimulation or inhibition of the sphincter of Oddi is often used to facilitate insertion of large duodenal papillary catheters (Tobuli et al. 1985).
It is not clear that because short-term pressure measurements do not accurately reflect the function of the sphincter of Oddi, possibly intermittent papillary stenosis. Abnormal papillary muscle function may not be detected during manometry of Oddi (Torsoll 1986). Long-term measurement of these parameters, thanks to the T-tube, shows similarly variable cyclic sphincter activity of Oddi. Duodenal activity between meals. The Oddi muscle contraction phase of 9-12 cycles/min lasts an average of 168 seconds (2-4 minutes), followed by phases of inactivity averaging 297 seconds (1-7 minutes). The normal increase in frequency of the sphincter of Oddi contraction rate was followed by 3 periods of silent, moderate, and increased frequency of about 76.5 minutes. Maximum contractile activity corresponds to phase III of the motor complex that moves between meals. Phase 1 corresponds to contractile inactivity. In phases I and II sphincter of Oddi activity is independent, in phase III sphincter of Oddi activity is closely related to duodenal contraction.
5. Opinions differ on the effect of cyclic sphincter of Oddi contraction on biliary drainage
According to some authors, cyclic sphincter of Oddi activity is peristaltic in nature leading to expulsion of bile into the duodenum (Toouli and Watts). According to some other authors, it is this activity that slows down the flow of bile and pancreatic juice. Very small probes are used to measure the sphincter of Oddi pressure on endoscopically, the pressure value is lower than the pressure value when measured with a cuff. Electromyography and pressure measurements show that the electrical activity of the sphincter of Oddi is rhythmic (due to an increase in action potential) corresponding to the ascending phase of the sphincter of Oddi pressure wave (Bortolotti 1985). Touli 1982 reported that there was no difference in sphincter of Oddi pressure between patients with gallbladder intact and patients with cholecystectomy. However, Tanaka, Ikeda and Nakayama 1984 performed an experiment that placed a super probe into the bile duct on 7 patients before and after cholecystectomy + sphincter induction with Morphin. Before cholecystectomy, morphine did not cause muscle weakness. Adding Carulein (Decapeptide 20 times stronger) contracts the gallbladder and increases bile duct pressure. The basal (baseline) pressure is also elevated after cholecystectomy, which means that the gallbladder has a role as a reservoir in pressure compromise.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: 1. Le Quang Quoc Anh. The basics of sphincterotomy of Oddi and endoscopic gallstone removal. Gastrointestinal diseases. Ho Chi Minh City Digestive Science Conference 1998, 35 - 40. 2. Le Quang Quoc Anh. Role of retrograde endoscopy in biliary-pancreatic pathology. Proceedings of the full text of scientific topics at the Vietnamese surgical conference. Surgical journal. Hue 2002, 61-70. 3. David Fleischer. Endoscopic management of biliary tract obstruction. Techniques in therapeutic endoscopy. Saunders 1992.8.2-8.7. 4. Franklin E. Kasmin, David Cohen, Subash Batra. Needle-knife sphincterotomy in a tertiary referral center: efficacy and complications. Gastrointestinal Endoscopy. Vol. 44, 1996, 48 - 53.