This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalPancreatic carcinoma (PDAC) carries significant morbidity and mortality and remains one of the most difficult malignancies to treat. Individual patient and tumor factors need to be taken into account to provide an optimal, personalized approach. The following article evaluates the response of pancreatic ductal carcinoma after adjuvant neoplasia
1. Evaluation of pancreatic ductal carcinoma response after neoplastic adjuvant therapy
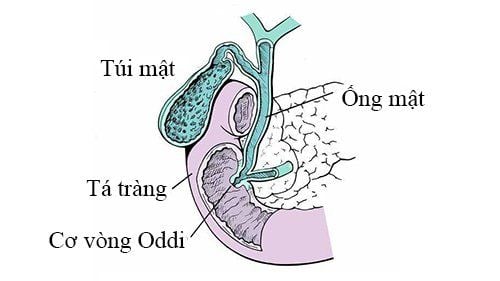
Conventional Ultrasound Abdominal (US) ultrasound is an economical and radiation-free investigation. It helps visualize diminishing pancreatic masses on unenhanced CT images. However, its role in the assessment of tumor response is very limited. However, US can be a useful tool to detect intra-abdominal complications and drug toxicity during the adjuvant treatment of neoplasia in metastatic pancreatic cancer. The most common adverse events of neoplastic adjuvant therapy for metastatic pancreatic cancer are neutropenic colitis and venous thrombosis, which are readily detectable by abdominal US .Endoscopic ultrasound Endoscopic ultrasound (EUS) has evolved from a mere imaging modality to one that allows tissue diagnosis through fine-needle aspiration. It has been shown to be a valuable means of early detection and staging of pancreatic carcinoma, especially for lesions ≤3 cm, superior to multi-detector CT. Recently, the role of EUS in providing adjuvant treatment of neoplasia in pancreatic ductal carcinoma and its response assessment is rapidly emerging. Das et al conducted a large sample study to investigate the value of EUS in predicting preoperative tumor response of pancreatic ductal carcinoma following adjuvant neoadjuvant therapy. The results show that tumor size change after neoplastic adjuvant therapy on EUS is a sensitive marker to assess tumor response, and tumor size reduction 47% is a factor. independent prognosis for survival in these patients.
A systematic review from Barreto et al compared the accuracy of imaging modalities to predict resectability and R0 resection for peritumoural contour or advanced pancreatic ductal carcinoma in situ after neoplastic adjuvant therapy. They show that effective imaging evaluation allows predictability of tumor resection. Furthermore, the decrease in tumor stiffness of pancreatic ductal carcinoma on tissue elastomer EUS can be used as a potential marker for neoplastic adjuvant response and assessment of resection potential. u. In addition, Figueedlyo et al. reported the role of EUS-guided technology in performing neoplastic adjuvant therapy for pancreatic carcinoma. The authors point out that EUS-guided placement of fiducial markers for stereosystemic whole-body radiation therapy in pancreatic ductal adenocarcinoma helped ensure the feasibility and safety of adjuvant therapy. next new born. The above studies illustrate the importance of EUS during adjuvant neoplastic treatment for pancreatic carcinoma.


Positron emission tomography 18F-fluorodeoxyglucose positron emission tomography (18-F-FDG-PET) is a diagnostic test that reflects the genetic, molecular, metabolic, and functional status of a lesion. The maximum standardized uptake value (SUVmax) obtained by PET imaging reflects the glucose metabolism of the tumours. Choi et al explored the relationship between early treatment response after neoplastic adjuvant chemotherapy with FDG-PET and surgical outcome in advanced pancreatic ductal carcinoma in situ.
CT perfusion Pancreatic ductal carcinoma is a matrix-rich tumor characterized by activation of pancreatic astrocytes, which deposit large amounts of extracellular matrix. The accumulation of extracellular matrix, including collagen, fibronectin, proteoglycan, and hyaluronic acid, can cause the formation of a stiff extracellular matrix to compress blood vessels, leading to perfusion injury and ultimately impeding delivery of anticancer drugs to tumor cells.

2. Structural analysis and data modeling
In recent years, many studies have emphasized the role of data visualization techniques in various aspects of pancreatic tumours, such as tumor characterization, assessment of surgical viability, etc. , risk of recurrence and predictability of survival. A previous study by Chen et al showed changes in CT radiographic features, such as imaging changes during chemotherapy, in patients with pancreatic carcinoma. The authors suggest that these alterations can be used for early assessment of treatment response and patient stratification to achieve precise and intensive treatment. Chakraborty et al conducted a preliminary study to investigate the value of CT texture analysis in quantifying tumor heterogeneity and predicting 2-year survival in patients with carcinoma. pancreas. The results suggest that CT texture features can predict heterogeneity in pancreatic tumours. At the same time, the accuracy of CT texture analysis in predicting 2-year survival rate can reach 82.86%. Therefore, it can be used to develop optimal treatment plans for pancreatic carcinoma patients.Recently, several studies have explored the utility of CT texture analysis in predicting operability and prognosis in patients with pancreatic ductal carcinoma and the relationship between texture features and the pathological response of the tumor. The results showed that CT texture characterization was more accurate in identifying tumors as resectable than unresectable. The authors conclude that pretreatment structural features of baseline CT images and longitudinal changes in tumor heterogeneity can be used as biomarkers to predict tissue response study with adjuvant chemotherapy and disease-free survival. In addition, Nasief et al. have reported the value of carbohydrate antigen 19-9 (CA19-9)-associated data visualization in the evaluation of neoplastic adjuvant therapy for adenocarcinoma. pancreas. The results showed that decreased CA19-9 levels and plain radiographic features were predictors of survival in these patients. The combination of delta-CA19-9 radioactivity features has the potential to increase adaptation to response-based treatment. It cannot be denied that data visualization or texture analysis has great promise in the management of pancreatic ductal carcinoma following adjuvant neoplasia. Current limitations of radiomics include time-consuming segmentation and uncertain conclusions. Further large-scale studies are needed to determine its true potential.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.