This is an automatically translated article.
Acute pancreatitis, a dangerous disease that can adversely affect life. Therefore, you should take the initiative to take care of and protect your health with a healthy lifestyle, diet and lifestyle. If there is a suspicion of signs of illness, it is necessary to visit a medical facility to be examined and apply supportive measures to treat acute pancreatitis.1. How dangerous is acute pancreatitis?
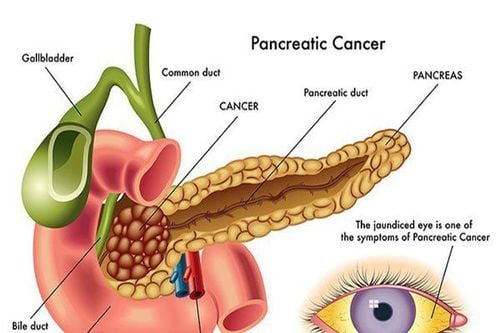
Acute pancreatitis causes destruction and fibrosis of the pancreatic parenchyma as well as widespread or localized damage to the pancreas. The process of fibrosis can cause widespread or localized calcification of the pancreatic duct, causing narrowing of the lumen of the pancreatic duct, leading to a decline in the endocrine and exocrine functions of the pancreas.Therefore, when the pancreas is damaged, its function is not guaranteed, and at the same time, it seriously affects the metabolism of substances in the body, which can cause dangerous complications.
One of the dangerous complications of pancreatitis is diabetes mellitus. Patients with pancreatitis cannot use sugar molecules in cell metabolism, leading to hyperglycemia.
Besides, the nutrients in food put into the body are not broken down and absorbed, so it will cause rapid weight loss leading to malnutrition and health failure.
Not only that, acute pancreatitis can also cause dangerous complications such as large pancreatic pseudocysts, blood clots in the veins or pancreatic cancer.
2. Treatment of acute pancreatitis
In case of severe acute pancreatitis and complications, it is necessary to intervene to treat acute pancreatitis and use antibiotics. In some specific cases, patients with acute pancreatitis may be indicated for surgical intervention such as: acute pancreatitis due to gallstones, pancreatic pseudocyst, pancreatic abscess, pancreatic necrosis, especially infectious necrosis. If the patient has acute pancreatitis caused by gallstones or gallstones, cholecystectomy may be considered within 7 days of recovery to reduce the risk of recurrence of acute pancreatitis. Treatment of severe and complicated acute pancreatitis usually includes: ICU care, sometimes artificial nutritional support, resection of necrotic foci, drainage of pancreatic pseudocyst...
Trong điều trị viêm tụy cấp người bệnh nên được bổ sung dịch sớm
3. Supportive treatment of acute pancreatitis
3.1 Fluid resuscitation Intravenous fluid resuscitation improves pancreatic perfusion, while also preventing potentially serious complications such as pancreatic necrosis.To treat acute pancreatitis, fluid should be added early, and given to all patients within the first 12 to 24 hours. However, for patients with cardiovascular disease, kidney disease or other related factors, this case does not apply. Adequate fluid resuscitation can be assessed by decreasing Hct and BUN indices within the first 24 h especially if acute pancreatitis is in the early stages.
Other parameters may improve vital signs and maintain consistent urine output. Fluid supplementation should be reassessed frequently during the first 6 hours of admission and during the next 24 to 48 hours. When patients with acute pancreatitis are resuscitated with fluid resuscitation, SpO2 should be measured, supplemented with oxygen as needed, and fluid inflow and outflow should be closely monitored.
Adequate fluid rehydration will prevent complications of acute pancreatitis, necrosis and improve organ failure in the body.
Isotonic or crystalline fluids are used to rehydrate patients with acute pancreatitis, the rate of compensation depends on the patient's fluid volume and cardiovascular status, about 250 to 300ml/hour for 48 hours for patients with acute pancreatitis. severe acute pancreatitis.
Vital signs, urine output (>0.5ml/kg/hour), CVP, Hct, and BUN are indicated every 12 to 24 hours to help assess fluid resuscitation.
Fluids should be continued in patients with acute pancreatitis until the risk of organ failure is assured.
3.2 Respiratory Care Maintain SaO2 >95%. 3. Metabolic balance Hyperglycemia should be treated carefully with insulin. Compensate for Mg and Ca when necessary. 3.3 Nasogastric tube insertion Not required in mild acute pancreatitis. Performed when there is a lot of vomiting, avoiding aspiration pneumonia and intestinal obstruction. 3.4 Nutritional support, functional preservation For mild acute pancreatitis: Patients with acute pancreatitis need fasting for the first few days, intravenous fluid replacement, patients usually eat again after 3-7 days. Patients with severe acute pancreatitis: Nutritional support is required, although the timing of initiation of support and the optimal duration of nutritional support remains unclear. However, using enteral nutrition and using parenteral nutrition only if enteral nutrition cannot be used helps maintain the intestinal mucosal barrier. Prevents intestinal dysentery that can occur when the intestines are inactive for a long time....

Giảm đau có vai trò quan trọng trong điều trị viêm tụy cấp
Effective pain relief requires intravenous opioids and appropriate dosage. In addition, antiemetics can also be used to relieve symptoms of nausea and vomiting in patients with acute pancreatitis.
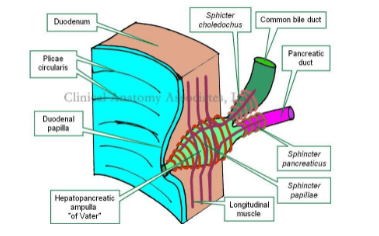
Pethidine (Meperidin) belongs to the first class of opioids 50-100mg every 4 hours. Fentanyl IV: Safe for mild acute pancreatitis even in the presence of renal failure, possibly with respiratory depression at doses of 20-50 μg for 10 minutes. Morphine and its derivatives may worsen pancreatitis by increasing the tone of the sphincter of Oddi. Anticholinergics such as atropin should be avoided in patients with acute pancreatitis due to exacerbation of intestinal obstruction. Acetaminophen will be indicated in mild acute pancreatitis or fever.
4. Monitoring and detecting complications of acute pancreatitis
How dangerous is acute pancreatitis? Injury to the liver and kidney sites can cause serious complications related to the respiratory system, circulatory system or multi-organ failure, which is considered the most serious complication of acute pancreatitis. Therefore, patients need to be actively monitored and promptly detected to have a timely treatment plan.Besides, it is also necessary to regularly monitor pulse indicators, blood pressure, body temperature, urine, blood oxygen saturation along with tests related to blood count, liver function, kidney function. electrolyte....
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.