This is an automatically translated article.
The article is professionally consulted by Master, Doctor Ta Quang Hung - Department of General Surgery - Vinmec International General Hospital Da Nang. The doctor has more than 10 years of experience in teaching and practicing in the field of Anesthesia.The procedure of endotracheal anesthesia in hepatobiliary surgery is a modern technique applied on hepatobiliary surgery patients to control the patient's respiratory function during and after surgery.
1. What is endotracheal anesthesia in hepatobiliary surgery?
Endotracheal anesthesia in hepatobiliary surgery is a technique of general anesthesia and endotracheal intubation for the purpose of controlling the patient's respiratory function during and after surgery.2. What preparation is required when performing endotracheal anesthesia in hepatobiliary surgery?
The team that performs endotracheal anesthesia in hepatobiliary surgery includes doctors and nurses in the specialty of anesthesiology and resuscitation.To perform the technique, the following tools and equipment are required:
Anesthesia machine system with breathing and oxygen source by hand squeeze Machine to monitor vital functions such as arterial blood pressure, breathing rate, ECG, EtCO2 , SpO2, temperature

3. Procedure for endotracheal anesthesia in hepatobiliary surgery
The procedure of endotracheal anesthesia in hepatobiliary surgery includes the following steps:Step 1: Place the patient in a supine position, install a monitor for vital functions, and establish an effective infusion. Before induction of anesthesia, give the patient 100% oxygen 3-6 l/min for at least 5 minutes. Pre-anesthesia can be performed if needed.
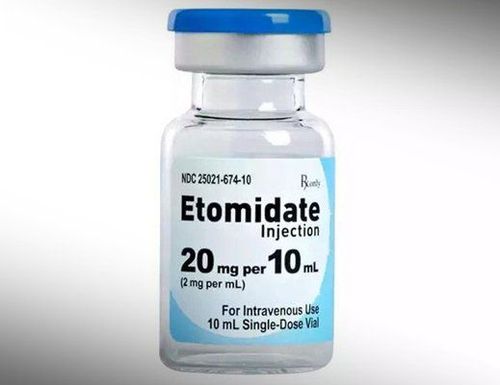
Step 2: Perform induction of anesthesia with drugs including sleeping pills that can be intravenous anesthetics (etomidate, ketamine, propofol, thiopental, ...), volatile anesthetics; pain relievers (fentanyl, morphine, fentanyl, ...); muscle relaxants (rocuronium, succinylcholine, vecuronium...) if needed.
Step 3: The condition for endotracheal intubation in hepatobiliary surgery is that the patient must sleep deeply enough and have enough muscle relaxation. Endotracheal intubation is performed as follows:
Open the patient's mouth, insert the laryngoscope into the right side of the mouth, use the tongue scraper to the left side to push the lamp deep, and at the same time use the table. Right hand presses the cricoid cartilage to find the epiglottis and glottis. In case the stomach is full (as soon as the patient loses consciousness begins to press the cricoid 20 - 30 kg until the endotracheal tube is complete), conduct rapid induction of anesthesia and perform the Sellick maneuver. The next step in the procedure of endotracheal anesthesia is to gently insert the endotracheal tube through the glottis until the balloon of the endotracheal tube passes about 2 - 3 cm through the vocal cords, then stops. Gently remove the laryngoscope and perform balloon intubation. Listen to the lungs to assess bilateral ventilation at 4 positions and see the results of 3 continuous waves of EtCO2 to check that the endotracheal tube position is correctly placed. Use adhesive tape to secure the endotracheal tube and place the cannula in the patient's mouth to avoid biting the tube when needed.
Step 5: Monitor the depth of the endotracheal anesthesia procedure with indicators including: blood pressure, heart rate, sweating, tearing (PRST); BIS, Entropy, MAC (if any)... Monitor vital signs on the machine including: blood pressure, heart rate, body temperature, EtCO2, SpO2. Care should be taken in case the endotracheal tube is placed in the wrong position, or the tube is bent or blocked.
Step 6: Remove the endotracheal tube when the patient is awake and able to follow orders. Raise the patient's head for more than 5 seconds, TOF > 0.9 (if present). The patient was breathing spontaneously and had a respiratory rate within the normal range. Blood pressure, pulse rate is stable, body temperature is over 35oC. The patient had no complications of anesthesia and hepatobiliary surgery.
4. Possible complications and management when performing endotracheal anesthesia in hepatobiliary surgery

Reflux of gastric juice into the airway: When detecting the patient has digestive juices In the oral cavity and airway, it is necessary to quickly drain the fluid, place the patient in a low position and tilt the head to one side. Promptly intubate the endotracheal tube and clear the airway. Monitor patients and prevent lung infections after surgery. Hemodynamic disorders: Depending on the symptoms and causes of disturbances in blood pressure (increase or decrease) and heart rate (fast, slow or arrhythmia) there will be appropriate treatment. Intubation is not possible in patients with hepatobiliary surgery: Switch to another method of anesthesia or apply difficult intubation procedures. Misplaced endotracheal tube into the stomach: Re-intubate the endotracheal tube when the lung is found to have no alveolar murmur and no EtCO2 can be measured. Vocal, air, and bronchial spasms: Quickly provide adequate oxygen to the patient, add hypnotics and muscle relaxants, and ensure ventilation and bronchodilators and corticosteroids in case of difficulty in ventilation. or not possible, auscultation with crackles or muted lungs. When respiratory function cannot be controlled during endotracheal anesthesia, a difficult intubation procedure should be used. Trauma when endotracheal intubation: Depending on the damage is tooth fracture, bleeding, foreign body falling into the airway, vocal cord injury, ... there will be appropriate treatment. Some respiratory complications such as a folded endotracheal tube, retraction deep into a lung, a collapsed or open respiratory system, depleted oxygen supply, or lack of oxygen due to expired soda: Quickly find the cause and resolve, and at the same time treat by providing 100% oxygen and ensuring ventilation. Some complications after extubation in hepatobiliary surgery patients such as respiratory failure, sore throat, hoarseness, vocal stenosis, trachea, upper respiratory tract inflammation: Depending on the cause and symptoms to treat suitable mind. At Vinmec International General Hospital, endotracheal anesthesia in hepatobiliary surgery is performed by a team of highly qualified and experienced doctors with modern equipment and operating rooms. meet international standards.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














