This is an automatically translated article.
The article was professionally consulted with Master, Doctor Ton That Quang - Head of Anesthesia - Anesthesia Unit - Department of General Surgery - Vinmec Nha Trang International General Hospital.Endotracheal anesthesia is an anesthetic method widely used in sclerectomy to treat cases of scleritis or glaucoma. This technique is performed according to standard procedures, ensuring a successful surgery, limiting possible complications.
1. Endotracheal anesthesia What is deep sclerectomy?
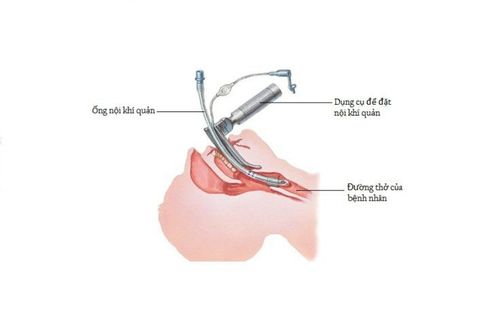
The sclera is the white part of the eye, the outer layer that protects the eye. The sclera occupies the posterior 4⁄5 of the eyeball. The sclera is prone to inflammation with a red sclera, which is painful for the patient. When the inflammatory process spreads from the sclera, it will lead to complications such as keratitis, peripheral corneal ulcer, corneal perforation, uveitis,...Anesthesia for deep sclerectomy is the method of choice. Anesthesia with endotracheal intubation (insertion of a catheter into the patient's trachea) aims at: Easy tracheobronchial aspiration; allow easy respiratory support; ensure the patient's breathing is stable during general anesthesia in positions, in critical stages as well as during post-operative resuscitation.
Indications for endotracheal anesthesia, deep sclerectomy is performed in patients with glaucoma (glaucoma); difficulty controlling the airway with a mask; necessitates maintenance of anesthesia with inhalational anaesthesia, for spontaneous breathing in infants and young children. Deep sclerectomy is contraindicated under endotracheal anesthesia if there are insufficient means of resuscitation or the performing physician is not technically proficient.

2. Procedure for performing deep scleral endotracheal anesthesia
2.1 Preparation
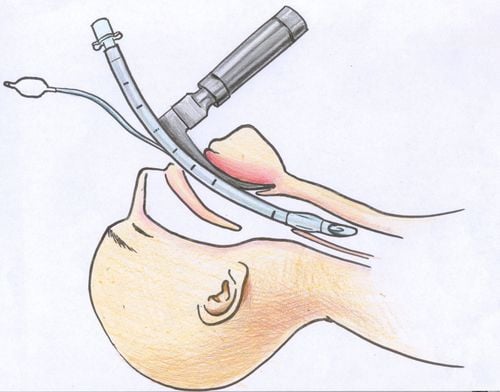
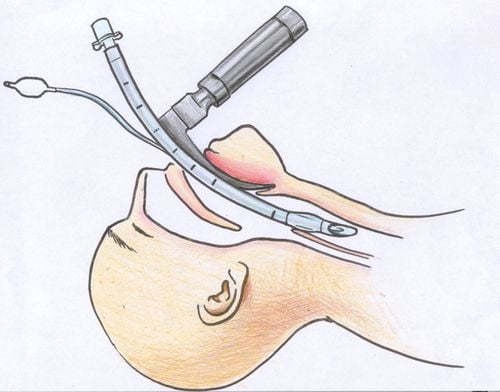
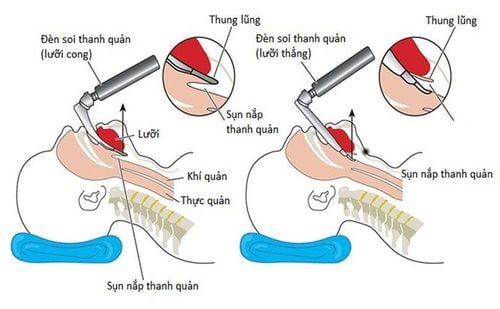
Personnel: Doctors and technicians specializing in anesthesiology and resuscitation; Technical facilities: Endotracheal lamp, endotracheal lamp blade, Magill pliers, soft mandrin, 10ml syringe, Guedel canul, endotracheal tube of various sizes, splint suitable for endotracheal tube, bronchoalveolar suction catheter mouthpieces and tubes, clean gloves, masks of all sizes, balloon system for manual respiration, Xylocain 5% dust spray, endotracheal tube fixation tape, eye protection tape, aspirator, ventilator, anesthesia machine, hand squeeze means, difficult intubation equipment; Patients: Be informed about the technique, procedure and risk of complications, guided to perform necessary procedures before starting anesthesia - surgery; Medical records: Prepare according to the regulations on necessary procedures.2.2 Technical implementation
Check records and patients; Prepare a stethoscope, measure pulse, blood pressure and aspirator; Pre-anesthesia: Use Atropin and Midazolam in appropriate doses; Using anesthetic drugs; Give the patient 100% oxygen first for a minimum of 3 minutes; Anesthesia: Usually begins with fentanyl, followed by a sedative and muscle relaxant. The dose of drugs used is calculated according to the dose of intravenous anesthetic; Insert the laryngoscope into the mouth, local anesthetic with xylocaine 5% spray. Spray the glottis 4 - 7 times, spray the larynx 4 - 7 times and spray the trachea 4 - 7 times. The number of sprays for 3 positions does not exceed 25 times; Perform the technique: Put the patient in supine position, place the head in the appropriate position as required when looking at the mouth, pharynx and larynx lying on a straight axis. The usual posture is the pillow 8 - 10cm high above the shoulder; The doctor uses the left hand to hold the laryngoscope, the right hand to open the patient's mouth (pay attention to widen the mouth), insert the lamp until the tip of the lamp is at the edge of the tongue - epiglottis; Raise the laryngoscope high, gently move forward, see the glottis. The doctor's right hand or the assistant's hand needs to press or push the thyroid cartilage slightly to the side to see the glottis; The doctor uses his right hand to insert the endotracheal tube into the right corner of each side, through the glottis; Stop pushing the tube when the balloon of the endotracheal tube passes about 2cm past the vocal cords; Use a 10ml syringe to inflate the balloon. The amount of air introduced is enough to no longer leak when breathing; Gently bring the laryngoscope out with the left hand; Hold the endotracheal tube close to the edge by clamping between the index finger and thumb of the right hand; Start manual respiration, check endotracheal tube position (by listening to 2 lungs, 2 axillaries); Evaluate SaO2 and EtCO2 values to determine the correct position of the endotracheal tube; Fix 2 tubes with 2 adhesive tapes; Place the cannula in the mouth to prevent the patient from biting the tube; Maintenance of anesthesia: The patient can be allowed to breathe on their own or breathe with command depending on the case; Let the patient breathe on their own with the evaporating anesthetic. Evaporative anesthetics are used, controlled through a special vessel; Breathe by machine or squeeze hands, maintain with inhalation anesthetic, combination anesthetic, fentanyl, muscle relaxant (interval or continuous infusion pump); Before the end of surgery, it is necessary to reduce the dose of intravenous anesthetic at the injection pump line and reduce the dose of volatile anesthetic; When using inhalational anesthetic, it is necessary to stop the drug at the end of surgery, open the valve to the fullest extent, increase ventilation and squeeze the reserve balloon to discharge the anesthetic during anesthesia; Monitor parameters while maintaining anesthesia including: Blood pressure, pulse, SaO2, EtCO2; Prevent the risk of endotracheal intubation, flexion or deep expulsion of the tube; Prevent nausea and vomiting in patients by using Ondansetron or Dexamethasone in appropriate doses; Criteria for extubation after endotracheal anesthesia: The patient is awake and can follow the doctor's orders: Open eyes, open mouth, stick out tongue, hold head high for 5 seconds, hold hands tightly; Breathe deeply and evenly without prompting; respiratory rate over 14 breaths/minute; tidal volume (Vt 8ml/kg); SaO2 index 98-100%; Stable pulse and blood pressure; If the patient does not meet the above criteria, it is necessary to evaluate the patient's condition, the effect of the muscle relaxant, the respiratory depression effect of Fentanyl, consider the patient still asleep due to the drug, can give the patient muscle relaxants or naloxone.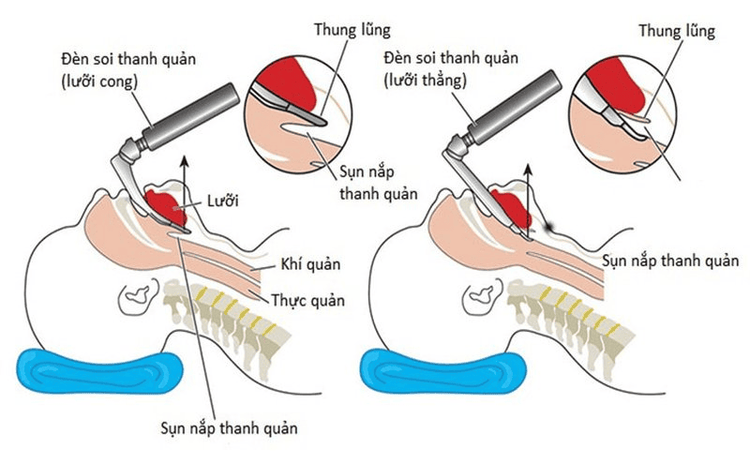
2.3 Extubation of endotracheal tube
Use a sterile straw 1 to clean the patient's throat and mouth; Aspiration of a nasogastric tube if placed; Remove the balloon of the endotracheal tube; Insert sterile suction tube 2 into the endotracheal tube, performing both suction and extubation.3. Some complications and handling measures
Pay attention to reflex complications during eye surgery such as bradycardia for appropriate management interventions.The procedure of endotracheal anesthesia for deep scleral resection is relatively complicated, so patients need to absolutely follow the doctor's instructions during the procedure to improve the possibility of successful treatment and reduce the risk of complications.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.