This is an automatically translated article.
This article is professionally consulted by Master, Doctor Hoang Thanh Nga - Ophthalmologist - Department of Medical Examination and Internal Medicine - Vinmec Ha Long International General Hospital.Glaucoma is often a common manifestation of glaucoma, but there is also a special case of primary glaucoma but intraocular pressure is within normal limits. Because the disease symptoms are not clear, it is difficult to detect. Although this disease does not cause high eye pressure, there are still irreversible eye injuries.
1. What is non-high pressure glaucoma?
Non-high pressure glaucoma is a type of primary open-angle glaucoma. In which, the patient presented with low intraocular pressure, but still had damage to the optic disc and visual field. Although the disease does not cause glaucoma, it still has serious effects on the patient's vision.Although it has the potential to cause irreversible vision loss, glaucoma manifestations are often minimal. If left untreated, the disease will progress to worse, vision will gradually decrease, eventually leading to irreversible blindness. The disease has a poor prognosis if accompanied by central retinal vein occlusion.
Glaucoma without high blood pressure does not have a clear pathogenic mechanism, but there are a number of related factors that increase the risk of disease such as:
Glaucoma is not high most of the patients are over 50 years old, usually It is more common in women than men, especially those with old age fibrosis, the incidence is higher. The disease is common in patients with vascular diseases such as hypertension, diabetes, high blood pressure. low blood pressure at night, vasospasm syndromes such as migraine, Raynaud's syndrome .... Family factors: It was found that some genes related to glaucoma are not high. Therefore, people who have a family member with the disease also need to pay attention to screening before the disease develops. Non-high pressure glaucoma is common in Asian countries, while black people have more high pressure glaucoma than other people of color.
2. Glaucoma symptoms are not high
Usually glaucoma is not high, has no symptoms or only blurred vision, so the disease is often discovered incidentally during eye examination or periodic physical examination, detecting signs of concave atrophy of the wide optic nerve while That is, intraocular pressure is within normal limits.However, in some late cases with severe eye damage, the symptoms are more obvious such as: Vision is decreasing, the field of vision is narrowing, even vision loss.
3. How to diagnose non-high pressure glaucoma?

Bệnh có ít triệu chứng lâm sàng, thường được phát hiện tình cờ khi khám mắt
Changes in intraocular pressure In patients with low-grade glaucoma, the intraocular pressure fluctuation and peak are less than 21 mmHg. It is necessary to chart the intraday intraocular pressure changes to confirm the diagnosis of non-high pressure glaucoma. It is now possible to monitor intraocular pressure at certain hours by using an electronic pen tonometer to monitor intraocular pressure.
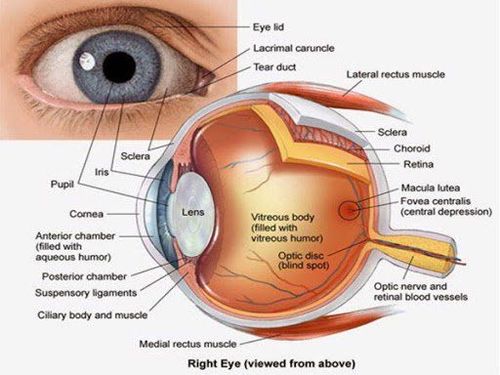
Optic spines Ophthalmoscopy shows damage to the optic disc with the same characteristics as other glaucoma such as: The border of the nerve around the optic nerve is thinner than that of high-pressure glaucoma. The papillae is not too deep, the ethmoid layer is less pushed back, the optic nerve border is often damaged in one location and accompanied by deep papillae concave, changing the ethmoid layer to form the papillomatous fossa. get.
When ophthalmoscopy finds other symptoms associated with low-pressure glaucoma, including:
Parapipular retinal atrophy (α and β areas), this is a common sign, this sign Not specific for non-high pressure glaucoma. Papillary hemorrhage: This is very common in non-high pressure glaucoma. Damage to the nerve fiber layer that is localized to a single site is more common than damage to the entire circumference of the optic disc. Look at the front corner of the room See the extended front room corners.
Laboratory tests Central corneal thickness is considered as a factor to evaluate intraocular pressure. In non-high pressure glaucoma, the central corneal thickness is thinner than normal, so the IOP is often lower than the actual IOP.
Test for disease risk factors: Need to monitor blood pressure 24 hours, for people with vascular disorders need to combine echocardiography.
Brain scan or magnetic resonance imaging is indicated if there is no match between visual impairment, visual field and papillae.
3.2 Differential diagnosis It is necessary to differentiate it from some diseases such as:
High pressure glaucoma has been treated: Ring disease has used drugs that have low eye pressure such as β-blockers, ACE inhibitors ... Glaucoma changes: This is an open-angle glaucoma disease caused by large fluctuations in intraocular pressure. When measured at low intraocular pressure, it is easy to mistake it for non-high pressure glaucoma. Chart the day's labels to confirm the diagnosis. Elevated intraocular pressure glaucoma that has been previously stabilized. Damage due to compression of the optic tract: When you see the spines, they become discolored, showing atrophy of the optic discs. Ischemic optic neuropathy: The optic nerve atrophy is seen as in glaucoma, in this case the field of vision is stable, without progress.
4. What should I do when I have non-high pressure glaucoma?

Điều trị glocom nhãn áp không cao chủ yếu là dùng thuốc
To meet the needs of patients for screening for eye diseases, Vinmec International Hospital currently provides Glaucoma Packages to help customers detect diseases early and have effective treatment, prevent dangerous complications.
Currently, Vinmec is implementing 2 packages of Glaucoma examination and treatment, including: Glaucoma early detection package and scleral trabeculectomy package to help:
Comprehensive eye examination and indication for surgery (if any) by experienced medical specialist. Counseling on drugs, food, factors that may affect surgery.. Anesthesia and resuscitation examination assesses the patient's general condition before surgery. Explain surgical prognosis. With 10 years of experience in the field of Ophthalmology, she used to work at Thai Nguyen Central Hospital and held the position of deputy head of the department and in charge of the Department of Ophthalmology at Thai Nguyen University of Medicine and Pharmacy. Master Hoang Thanh Nga has a lot of experience in the field of examination and treatment of eye diseases. Currently, he is an Ophthalmologist at the Department of General Internal Medicine, Vinmec Ha Long International General Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
SEE ALSOGlaucoma (predominantly common): How is it diagnosed and treated? Examine the anterior angle of the room to assess the condition of the anterior chamber. Can glaucoma and glaucoma be operated on?