This is an automatically translated article.
The article is professionally consulted by Master, Doctor Huynh Khiem Huy - Cardiac Resuscitation Doctor - Cardiovascular Center - Vinmec Central Park International General HospitalAcute cardiac tamponade is an acute condition in which the heart is compressed due to the accumulation of fluid (or blood, pus) in the pericardial cavity, causing hemodynamic consequences ranging from mild cardiovascular collapse to severe cardiogenic shock and death. death if not treated promptly.
1. Symptoms of acute cardiac tamponade
1.1 Clinical The patient has clinical symptoms such as increased venous pressure causing varicose veins, abdominal pain, nausea, vomiting. In addition, patients have difficulty breathing due to decreased cardiac output, decreased lung volume due to enlarged heart, pleural effusionChest pain, fever, accompanied by chills, shock, cold, skin sweat, blood pressure hypotension, impaired consciousness, systolic blood pressure difference ≤ 80 mmHg, urine < 20 ml/h, blood pressure difference < 20 mmHg.
Actual symptoms may be observed in patients with inspiratory inversion whose systolic blood pressure falls by more than 10 mmHg, or by a 50% decrease in systolic pressure amplitude compared with expiration. This is a very important symptom of acute cardiac tamponade. When patients have arrhythmia, severe hypotension, it is difficult to detect.
In addition, the patient has symptoms of hepatomegaly, edema, thin heart, weakness, or loss of heart rhythm, if there is little fluid, there is a pericardial rub. Central venous pressure is always elevated during chest compressions, except when acute pericardial hemothorax is due to trauma, during the first few minutes central venous pressure has not increased because of blood loss. The jugular vein is distended and pulsating in the sitting position, reflecting central static pressure.
1.2 Subclinical Through subclinical diagnostic methods can quickly detect acute cardiac tamponade such as:
Electrocardiogram: sinus tachycardia, low voltage, non-specific ST-T changes Echocardiographic sign: shows right atrial–right ventricular collapse during diastole, heart dancing (shaking) in the fluid-filled pericardial space Straight chest X-ray without any X-ray symptoms decide whether to have acute tamponade, show only the images of pericardial effusion: enlarged heart, vial or spherical

Đau ngực dữ dội là một trong những biểu hiện của chèn ép tim cấp
2. Diagnosis of acute cardiac tamponade
Pericarditis due to infectious pathology; Pericarditis in systemic autoimmune diseases; Pericarditis due to type 2 (auto)immune process; Pericarditis and pericardial effusion in the setting of related organs; Pericarditis in metabolic disorders; Traumatic pericarditis; Pericardial disease due to cancer. Special cardiac tamponade syndromes:Localized cardiac tamponade; Cardiac tamponade with left ventricular failure; Low pressure cardiac tamponade.
3. Emergency cardiac tamponade
The principle of emergency cardiac tamponade should be urgently by prompt aspiration of pericardial fluid by puncture or surgical drainage. The cause of acute cardiac tamponade should be treated aggressively.Emergency cardiac tamponade can be performed by medical treatment or surgical intervention.
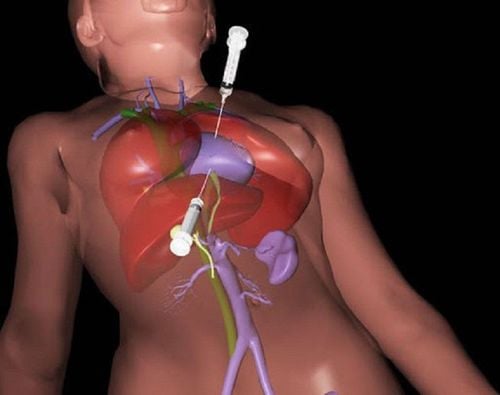
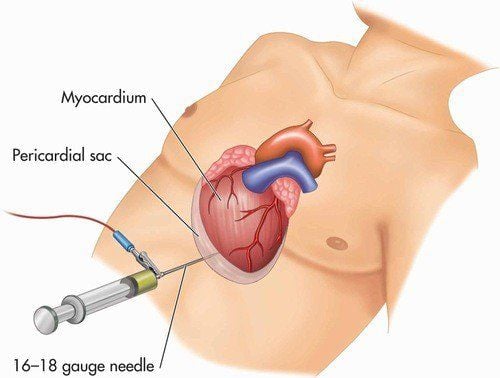
3.1 Interventional pericardiocentesis Indications:
Mild CET, not rapidly progressing: clinical monitoring. Moderate to severe CET: elevation of central venous pressure 10 mmHg or more or arterial blood pressure. Systolic < 100 mmHg: remove the fluid by aspiration or by surgical methods. Instruments:
18 needle (for rapid aspiration – aspiration of thick, viscous fluid) or Cavafix catheter or Sertofix catheter; Prong 3 (for aspiration, removed and attached to a manometer to measure pressure in the pericardial cavity); Syringe 25mL or 50 mL; The monitor monitors the heart rate continuously during the puncture; Electrocardiogram attached to the needle (alligator electrode) to check the needle tip position makes the procedure safer. Technique and location of punctures :
Methods: there are two methods + Pericardial puncture under the guidance of fluorescent screen
+ Pericardial puncture under ultrasound guidance
Dieulafoy line: location puncture: In the V intercostal space – 1-2 cm outside the apex, towards the spine. Marfan line: puncture site: just below the sternum blade, needle direction: Towards the left or right shoulder. Preferably due to avoidance of the pleura and major coronary arteries and more favorable aspiration puncture Any needle position and direction: follow ultrasound guidance for maximum drainage. Number of punctures:
Unlimited: If there is a lot of fluid, after manual aspiration to decompress, a continuous drainage should be placed to avoid withdrawing too much fluid (usually the drainage rate should not exceed 1 ,5 l/24h). Remember: the closer to the end of the procedure, the higher the risk of the needle tip touching the pericardial wall. 3.2 Analysis of pericardial fluid Meaning: can help diagnose the cause of pericarditis: tuberculosis, fungus, cholesterol, malignancy... However, which pericardial fluid test to choose to should be based on clinical manifestations. Tests for specific etiologies: + Cancer: cytological and oncological markers: CEA, AFP, carbohydrate antigen CA 125, CA 72-4, CA 15-3, CA 19 - 9, CD – 30, CD – 25...
+ Tuberculosis: AFB staining (acid-fast bacilli), bacterial culture, ADA (adenosine deaminase), gamma interferon, pericardial lysozyme, TB PCR (specificity 100 %).
+ Germs: Inoculate pericardial fluid with at least 3 samples, in aerobic and anaerobic environments. Blood cultures should be taken at the same time as fluid cultures.
+ Virus: PCR testing of some common viruses can help differentiate from self-reactive pericarditis.
Some other tests: + Biochemistry: Determine density, protein, LDH, glucose, permeation or exudate. Protein, LDH, and blood glucose should be tested at the same time.
+ Cells and blood cell formula: polymorphonuclear leukocytes, lymphocytes, mononuclear BC
...
+ Malignant cells.
+ Cholesterol.
Complications of puncture :
Touching adjacent structures: liver - pleura - coronary artery - right ventricle. Sudden death.
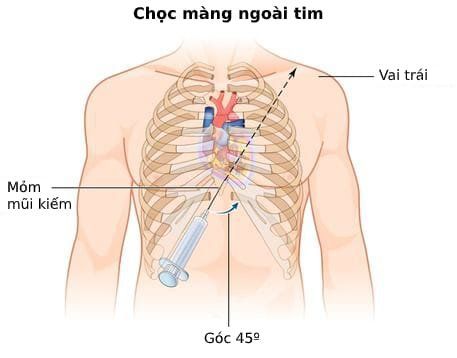
Chọc dịch màng ngoài tim cấp cứu chèn ép tim cấp
Resuscitation: if pulse collapse or severe shock + O2 breathing
+ Vasopressors: Dopamine 2 - 20mcg/kg/min - IV (adjusted dose depending on blood pressure)
Contraindicated treatments: drugs to reduce preload , varicose veins, diuretics, blood injections. Treat the cause: if identified. Other measures: (in case of difficult, ineffective aspiration): opening the pericardial window, pericardectomy. 3.4 Treatment after emergency cardiac tamponade Monitor for signs of recurrence; Diagnose the cause and treat it thoroughly; Detect comorbidities; The catheter can be kept for 48-72 hours for continuous drainage or for drug therapy; The catheter is usually removed within 24-48 hours to avoid the risk of infection.
4. Prevention of recurrent cardiac tamponade
In most cases, standard drainage is sufficient to avoid recurrence.After 03 days of standard drainage: if the drainage continues > 300ml/24h, more aggressive treatment should be considered. Methods of preventing pericardial fluid re-establishment: sclerosing agents (tetracyclines, non-absorbable steroids); chemotherapy; opening the pericardial window with a percutaneous balloon; surgical intervention. Pericardial fluid re-establishment with cardiac tamponade: surgical intervention should be considered. To protect cardiovascular health in general and detect early signs of cardiovascular disease, customers can sign up for Cardiovascular Screening Package - Basic Cardiovascular Examination of Vinmec International General Hospital. The examination package helps to detect cardiovascular problems at the earliest through tests and modern imaging methods. The package is for all ages, genders and is especially essential for people with risk factors for cardiovascular disease.
Master. Dr. Huynh Khiem Huy has more than 11 years of experience working in the field of cardiovascular resuscitation anesthesia; examination and resuscitation treatment after surgery for cardiovascular diseases in adults and children. Dr. Huy was former deputy head of the Department of Surgical Resuscitation at Tam Duc Heart Hospital before being a cardiothoracic resuscitator in Cardiovascular Surgery, Cardiology Center - Vinmec Central Park International General Hospital
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.