This is an automatically translated article.
To diagnose acute malnutrition, nutritionists rely on one of two criteria: arm circumference or weight-to-height ratio. In addition, children with acute malnutrition also have other clinical manifestations such as nutritional edema.
1. What is acute malnutrition?
Acute malnutrition is a condition in which meals do not meet the body's needs for energy and protein, leading to deficiency and causing rapid weight loss or swelling in children.
If suffering from acute malnutrition, especially severe, children may face a higher risk of death than children of normal development, this rate can be up to 5 - 20 times. Acute malnutrition is also known as a direct cause that can lead to death or an indirect cause that increases the risk of death, especially in the case of children suffering from diseases such as diarrhea, pneumonia.
2. Diagnostic criteria for acute malnutrition
There are 2 criteria used to diagnose acute malnutrition, which are:
Arm circumference measurement Weight-to-height ratio Children are diagnosed as acute malnutrition when 1 of 2 criteria This is lower than the threshold. In addition to these two criteria, combined with specific clinical manifestations, acute malnutrition is classified as moderate or severe.
2.1. Criteria for diagnosis of acute moderate malnutrition Children have moderate acute malnutrition when anthropometric indices and the following manifestations:
Arm circumference: Between 115 and 125mm (used used in the diagnosis of children 6 months of age and older and less than 5 years of age). Weight to height ratio: From -3SD to -2SD. Clinical manifestations: unclear, discreet, easy to ignore and not detected in time.

Suy dinh dưỡng cấp tính mức độ vừa cần được phát hiện sớm
2.2. Criteria for diagnosis of severe acute malnutrition Children with severe acute malnutrition have anthropometric indices and the following manifestations:
Measurement of arm circumference: Less than or equal to 115 mm. Weight to height ratio: Less than -3SD. Clinical manifestations: Depending on the type of malnutrition, children will have different manifestations, including edematous, atrophy or suitable.
3. Severe forms of acute malnutrition
3.1. Acute malnutrition with edema Diagnose acute malnutrition with severe edema when the child has the following clinical signs:
Nutritional edema: The child has edema from 2 or more lower extremities to the whole body. The two sides of the body have the characteristics of uniform swelling, white skin, when pressed, the skin feels soft and concave. Nutritional edema is used as the diagnostic criterion for acute malnutrition in children and differentiates it from edema caused by other causes. Pneumonia or digestive system disorders (often accompanied) Skin pigmentation disorders: Children with acute malnutrition may have edema characterized by red spots on the buttocks and around the anus, groin and extremities, concentrated in patches, after time, the red spots darken and peel off, infecting the skin. Osteoporosis due to lack of calcium and vitamin A in children. Enlarged liver due to fat loss. Heart failure due to protein deficiency. The test indicators decreased such as: hemoglobin, hematocrit, protein, prealbumin, sodium, potassium, blood sugar, ... 3.2. Acute malnutrition atrophy Diagnose a child with severe acute malnutrition if the following symptoms are present:
The child is thin, emaciated, eyes sunken inward, skin is dry, wrinkled due to fatty layer under the skin of the face, extremities and buttocks are absent. Manifestations of vitamin A, B1, B2, D, K deficiency... No appetite. Laboratory indicators decreased: Hemoglobin, hematocrit, blood protein, prealbumin, blood sugar, electrolytes.
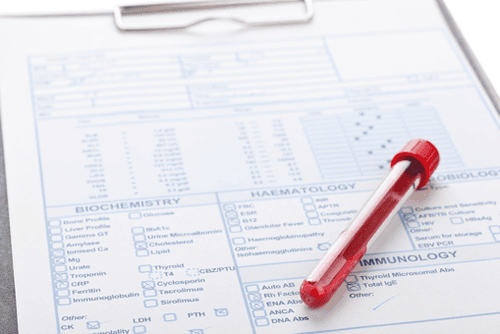
Suy dinh dưỡng cấp tính thể hiện qua các kết quả xét nghiệm
Acute malnutrition with combined severity is recognized through the clinical manifestations of both edema and atrophy mentioned above. Combined with diagnostic criteria for acute malnutrition and clinical manifestations to assess the extent and determine the type of malnutrition. Ideally, when children have health problems, parents should take their children to medical facilities to be examined by a doctor, in order to have timely interventions, to ensure good health and development of children. .
To prevent and improve malnutrition in children, parents should supplement with supporting products containing lysine, essential micro-minerals and vitamins such as zinc, chromium, selenium, B vitamins to help meet meet the nutritional needs of children. At the same time, these essential vitamins also support digestion, enhance nutrient absorption, help improve anorexia, and help children eat well. Parents can also apply dietary supplements and functional foods derived from nature for easy absorption by the baby. The most important thing is that the improvement of the baby's symptoms must take place over the long term. Combining many types of functional foods at the same time or changing many types in a short time can make the baby's digestive system unable to adapt and completely not good. Therefore, parents must be really persistent with their children and regularly visit the website vimec.com to update useful baby care information.