This is an automatically translated article.
Diabetic eye damage is a common dangerous complication. Therefore, to limit the risk of complications, people with diabetes need to control blood sugar and exercise well.
1. What does diabetic eye damage include?
Eye complications are one of the most common complications of diabetes. The longer the disease is present, the higher the risk of eye disease. In addition, a number of other factors also increase the risk of eye complications including:
High blood pressure Kidney failure Pregnant women Obese people Smoking The main eye damage caused by diabetes includes retinopathy. , Cataract . In addition, some other eye diseases can also be encountered such as chalazion, stye, blepharitis, dry eye, glaucoma, ophthalmoplegia.
To limit the risk of eye diseases caused by diabetes, patients need to have good control of blood sugar, a balanced diet and exercise, and maintain a healthy lifestyle.

Tăng huyết áp góp phần tổn thương mắt do đái tháo đường
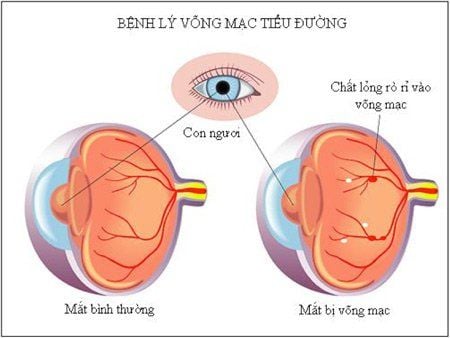
2. Diabetic retinopathy
Diabetic retinopathy occurs due to an imbalance between endothelial and parietal cells. Congested and enlarged capillaries lead to hyaline phenomenon, forming arterioles and venules causing gradual narrowing of the lumen. When the microvasculature is completely blocked, the ability to supply oxygen is reduced, causing endothelial and parietal cells to be destroyed.
Cell swelling occurs due to accumulation of sorbitol causing increased osmotic pressure. Sorbitol accumulation is due to high blood glucose levels, which are metabolized by the alcohol-forming pathway. Hypoxia in the retina occurs when cells become enlarged, reducing their ability to diffuse oxygen. Hypoxia and damage to capillary endothelial cells increase capillary permeability leading to retinal edema, formation of hard exudates, and retinal hemorrhages.
Common symptoms in diabetic retinopathy are blurred vision, distorted vision, flying flies, and color disturbances. Retinopathy is identified by a number of laboratory tests such as fluorescein angiography, retinal color imaging.
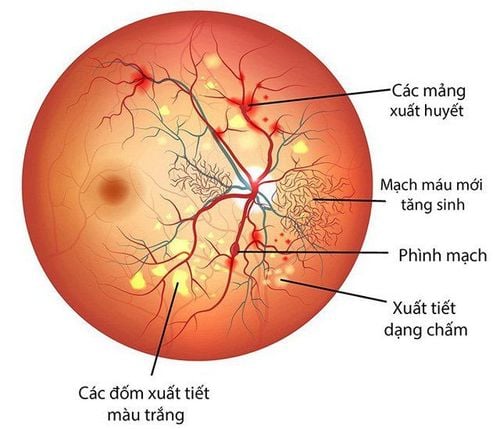
Retinal lesions are divided into the following stages:
Mild non-proliferative: Only presence of microaneurysms Moderately nonproliferative: Presence of microaneurysms with at least one Among the signs are punctate retinal hemorrhages, hard exudates, and soft discharges. No severe proliferative: There are signs of moderate stage accompanied by at least one of the signs such as retinal hemorrhage in more than 1⁄4 retina; bead veins on 1⁄2 retina; retinal microvascular abnormalities on 1⁄4 retinas; There were no signs of vascular proliferation. Proliferative: Signs of a severe proliferative phase accompanied by at least one sign of retinal neovascularization; vitreous haemorrhage/preretinal haemorrhage.
Bệnh võng mạc đái tháo đường
3. Diabetic Cataract
Diabetic cataracts are caused by a decrease in plasma concentration in the aqueous humor which leads to hydrolysis of the vitreous and eventually to opacity.
The main cause is thought to be due to increased blood glucose concentration causing glucose to diffuse into the vitreous. Some of the glucose is converted to sorbitol. Sorbitol is not metabolized but accumulates in the lens and penetrates the vitreous fibers causing fibrosis and cataracts. In addition, sorbitol also disrupts osmotic pressure, increasing water absorption into the vitreous fiber. The polyol process also releases many free radicals that cause damage to the lens. In addition, high intracellular concentrations of sorbitol in epithelial cells accelerate apoptosis. High concentrations of glucose in the aqueous humor cause glycation of proteins to produce vitreous toxic products. These processes combine to cause cataracts in diabetic patients.
Common symptoms of diabetic cataract include:
Early stage: There are almost no abnormal vision symptoms. Advanced stage: Some common symptoms include: Blurred vision, images darken but no pain Colors are lighter than before or slightly yellowing Sensitivity to light (dazzle) Difficulty seeing at night at night or in a place with insufficient light One-to-two vision in one eye Must change eyeglasses more often

Một số cấp độ của bệnh đục thủy tinh thể
4. Some other eye complications related to diabetes
4.1 Chromatosis occurs due to blockage or stagnation of secretions in the Meibomius gland. The disease is also known as chronic inflammatory granulomatous inflammation - fat. Cleft is a hard mass on the eyelid, painless, well-defined, the external skin is almost normal, inflammatory signs are not prominent.
4.2 Stimulants are abscesses - abscesses caused by infections, blocked ducts in the skin usually caused by bacteria Staphylococus Aureus. Prominent inflammatory signs include swelling, redness, pain, and swelling of the eyelid margins, irritation causing congestion and conjunctivitis of the cornea, and possibly white or yellow pus spots on the eyelid margins or under the conjunctiva of the eyelids.
4.3 Dry eye Dry eye occurs due to decreased sensation of the ocular surface causing decreased tear secretion reflex accompanied by dysfunction of ocular surface epithelial cells.
Tình trạng khô mắt
4.4 Neovascular glaucoma Neovascular glaucoma is secondary glaucoma due to abnormal development of new vessels on the iris, these new vessels obstruct the drainage of aqueous outflow of the eye causing glaucoma. The iris neovascularization is a fibrovascular membrane, initially fibrovascular tissue covers the open anterior chamber angle, over time this tissue shrinks causing anterior circumferential adhesion and causes angle closure. The cause of iris neovascularization in diabetic patients is ischemic, so neovascular glaucoma can be considered a complication of diabetic retinopathy and central retinal vein occlusion.
5. Diagnosing eye damage caused by diabetes
5.1 Ultrasonography Ultrasonography provides a preliminary view of the structure of the eyeball, especially in a transparent medium where light-based imaging cannot identify the disease. Ultrasonography also helps predict increased intracranial pressure with a sensitivity of up to 90% when measuring the diameter of the optic nerve sheath.
5.2 Fundus color photography Photographing fundus color helps to observe the parts at the fundus including retina, retinal blood vessels, optic spine, fundus abnormalities. Take several times in the case of monitoring the disease progression of the fundus. However, the test results are only qualitative, not detecting microscopic lesions.

Siêu âm mắt giúp chẩn đoán bệnh lý
5.3 Fluorescent retinal angiography Fluorescent retinal angiography provides detailed visualization of retinal vascular structures, neovascularization, aneurysms, blood flow, and permeability abnormalities. Because the technique is complicated, penetrating into the body can cause complications, it should not be performed in severe, uncooperative patients.
The technique is performed by injecting fluorescein dye into the arm vein. Wait a short time, when the dye has moved to the blood vessels in the eye, take the picture. The scanner has a special light filter that is sensitive to the dye present in the blood vessels at the back of the eye.
5.4 Retinal tomography Retinal tomography is a non-invasive, high-resolution technique that helps to observe microscopic lesions, measure and diagnose retinal lesions early. However, this is a costly test and cannot be performed when the medium is poorly transparent.
Diabetic eye damage is one of the complications that is not uncommon but has a significant impact on eye health. Therefore, when having diabetes, in addition to good control of blood sugar, patients also need to have regular health check-ups to avoid damage and complications of the disease from spreading to other parts.
To register for treatment or learn about eye surgeries performed at Vinmec International General Hospital, customers can contact Vinmec Health System nationwide, or register online HERE HERE