This is an automatically translated article.
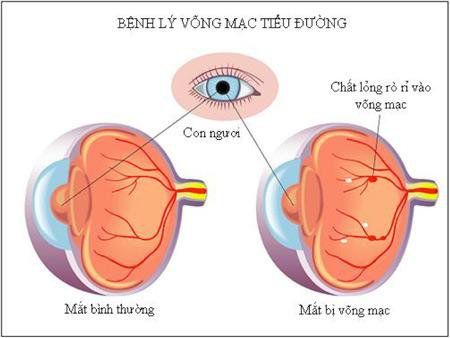
Posted by Master, Doctor Bui Minh Duc - Head of Department of General Internal Medicine - Department of General Internal Medicine - Vinmec Times City International HospitalDiabetic retinopathy often affects both eyes, and it is important to ensure that the risk of vision loss is minimized by accurately diagnosing the condition and taking timely treatment interventions.
1. What is diabetic retinopathy?
Diabetic retinopathy is damage to the retina from complications of diabetes, which is the leading cause of blindness in the United States. This condition can lead to blindness if left untreated. Early blindness from diabetic retinopathy is often preventable with routine screening and effective management of the underlying diabetes.
2. What are the symptoms of diabetic retinopathy?
Diabetic retinopathy often has no symptoms in the early stages, when in the advanced stage, symptoms begin to appear, in some cases, the patient has only 1 symptom, which is sudden vision loss. abrupt and complete.
Some of the signs and symptoms of diabetic retinopathy may include:
Blurred vision Impaired color vision Dark spots like “Fly”- cloudy or transparent and colorless spots and dark spots floating in the patient's vision Patches or streaks obstructing the patient's vision Poor night vision Sudden and total loss of vision Diabetic retinopathy usually affects both eyes Patients need to be assured that the risk of vision loss is minimized. The only way that people with diabetes can prevent diabetic retinopathy is to follow any eye exams scheduled by their doctor.
3. Causes and risk factors for diabetic retinopathy?
Damage to the network of blood vessels that nourish the retina is the main cause of diabetic retinopathy. In addition, anyone with diabetes is at risk of developing diabetic retinopathy. However, there are more risks if the patient has factors such as:
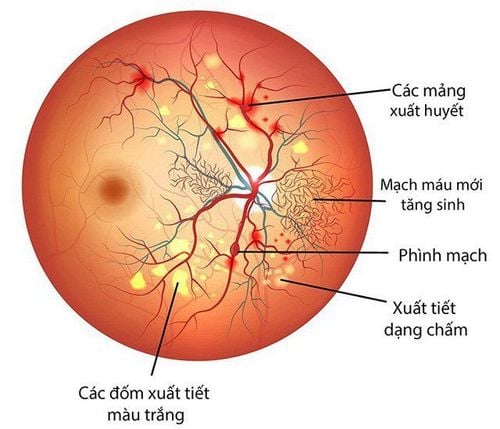
Not well controlled blood sugar Having high blood pressure Having hyperlipidemia Pregnant Smoking regularly Having diabetes for a while Long-term High glucose levels damage blood vessels and restrict blood flow to the retina. Blood vessel problems can be as mild as small bulges in the walls of blood vessels that occasionally leak blood without affecting vision. However, in advanced stages of the disease, these blood vessels can become completely blocked. Then, the fundus produces less stable neoplastic blood vessels. New vessels are prone to rupture and leak into the vitreous of the eye. Bleeding causes blurred vision and further narrows the retinal blood vessels. Sometimes, this bleeding forms scars that can separate the retina from the eye, leading to retinal detachment. As symptoms develop, people with diabetic retinopathy are increasingly likely to experience complete vision loss.
4. Complications of Diabetic Retinopathy
Possible complications associated with diabetic retinopathy include:
Vitreous hemorrhage: A newly formed blood vessel leaks into the vitreous, filling the eye, preventing light from reaching the retina. Symptoms include loss of vision and sensitivity to light or vitreous cloudiness in milder cases. This complication may resolve on its own if the retina remains undamaged. Retinal detachment: Scar tissue can pull the retina away from the back of the eye, often causing the appearance of vitreous clouding points in the patient's vision, causing glare and severe vision loss. If the retina is detached, there is a risk of total vision loss if left untreated. Glaucoma: The normal flow of fluid in the eye can become blocked as new blood vessels form. The blockage causes glaucoma, which increases the risk of optic nerve damage and vision loss.
5. How is Diabetic Retinopathy Diagnosed?
Diabetic retinopathy usually begins without any noticeable change in vision. However, an ophthalmologist or ophthalmologist can spot these signs. It is important for people with diabetes to have an eye exam at least 1 to 2 times per year, or as recommended by their doctor.
Diabetic retinopathy can be diagnosed using optical tomography (OCT). In addition, some other methods may be indicated including:
5.1 Eye exam with pupil dilator drops The doctor puts drops in the patient's eyes, these drops dilate the pupils and allow the doctor to see closer to the inside of the eye in more detail. The photos are taken inside the eye. During an eye exam, your doctor may detect the presence of:
Abnormalities in blood vessels, optic nerve or retina Cataracts Changes in eye pressure or overall vision New blood vessels Retinal detachment Scar tissue Pupil dilators can be irritating, and the glare of the images can startle the patient. In people at high risk, eye drops can increase eye pressure.

5.2 Fluorescein angiography Drops are used to dilate the pupils and a special dye called fluorescein is injected into a vein in the patient's arm. Images are taken as the dye circulates through the eye. The dye can leak into the retina or leave marks if the blood vessels are abnormal.
This test can determine which blood vessels are blocked, secreted, or broken. The results are then used to accurately guide laser treatments. For about 24 hours after the test, the skin may turn yellow and the urine dark orange as the dye leaves the body.
5.3 Optical coherence tomography (OCT) This non-invasive scan provides high-resolution cross-sectional images of the retina, showing its thickness. Scans can be used to assess the effectiveness of any treatment.
After any treatment, then OCT is similar to an ultrasound test but uses light instead of sound to create images. The scan can also detect diseases of the optic nerve.
6. What are the treatment options for diabetic retinopathy?
Treatment of diabetic retinopathy depends on several factors, including the severity and type of diabetic retinopathy, and the patient's response to previous treatments.
With non-proliferative diabetic retinopathy, the doctor may decide to closely monitor the person's eyes without intervention. This is called watchful waiting. Patients need to work with their doctor to control their diabetes. Good control of blood sugar can significantly slow the development of diabetic retinopathy.
In most cases, proliferative diabetic retinopathy requires immediate surgical treatment. The following options may be available:
Focus laser treatment (Focal laser) The procedure is done in a doctor's office or an eye clinic. Targeted laser ablation will seal leaks from abnormal blood vessels. Photocoagulation can stop or slow the discharge and bleeding of the fundus.
Patients will usually experience blurred vision for 24 hours after focusing laser treatment. Small spots may appear in the vision for several weeks after the procedure.
Scattered laser treatment Total retinal laser ablation is applied to areas of the retina distal to the macula, usually using 2 or 3 courses. The macula is the area in the center of the retina where vision is strongest. Laser ablation causes new blood vessels to contract abnormally and form scars. Most patients require 2 or 3 courses for best results. Patients may experience blurred vision for 24 hours after the procedure and may experience loss of night vision or peripheral vision.
Vitrectomy The surgeon removes part of the vitreous inside the eyeball. The surgeon replaces the cloudy vitreous with a clear liquid or gas. The body will eventually absorb the gas or liquid, helping to create new vitreous to replace the damaged vitreous that was removed.
Hematoma in the vitreous and scar tissue pulling up the retina will be removed. This surgery is done in a hospital under general or local anesthesia.

The retina can also be strengthened and held in place by small forceps. After surgery, the patient may have to wear an eye patch to gradually use the eye again, which can cause fatigue after vitrectomy.
If gas is used to replace the removed vitreous, the patient should not fly until all the gas has been absorbed into the body. The surgeon will tell the patient how long it will take to fly. Most patients will experience blurred vision for several weeks after surgery. It can take several months for normal vision to return.
Surgery is not a cure for diabetic retinopathy. However, it can stop or slow the progression of symptoms. Diabetes is a long-term condition where damage to the retina and subsequent loss of vision can still occur despite treatment.
7. How to prevent diabetic retinopathy?
For many people with diabetes, diabetic retinopathy is a corollary. However, diabetics who successfully control their blood sugar will help prevent the onset of severe diabetic retinopathy.
High blood pressure is another risk factor. People with diabetes need to control their risks, including high blood pressure, by:
Having a healthy and balanced diet Regularly exercising Maintain a reasonable body weight Avoid smoking / quit smoking Strictly control alcohol intake Practice blood sugar and blood pressure control as directed by your doctor Follow regular screening appointments Detecting symptoms early will increase the effectiveness of treatment for retinopathy. diabetes.
At Vinmec International General Hospital, we always deploy a screening package for diabetes and dyslipidemia to help detect pre-diabetes early, accurately classify diabetes type, develop a nutritional regimen, monitoring to minimize the risk and complications caused by diabetes.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
MORE
What is retinopathy? What are the common types? Common diseases of the cornea Beware of hypertensive retinopathy