This is an automatically translated article.
Article by Doctor, Doctor Hoang Minh Duc - Vinmec Stem Cell Research Institute and Gene Technology
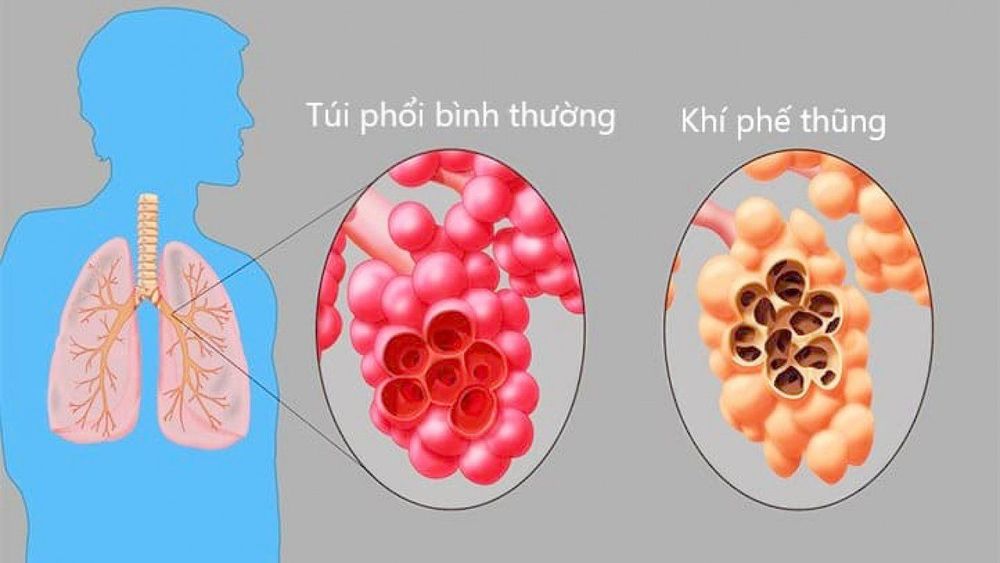
Chronic obstructive pulmonary disease (COPD) is a common disease, characterized by persistent airflow limitation, progressive disease, and often associated with a chronic inflammatory response in the airways and parenchyma lungs due to harmful particles and gases. Exacerbations and comorbidities contribute to individual aggravation.
According to the Global Burden of Disease Assessment report, the estimated number of COPD cases in 2015 was 174.5 million cases, an increase of 44.2% compared to 1990. The number of deaths due to chronic obstructive pulmonary disease is about 3.2 million worldwide. world, ranked 4th among the top 10 causes of death in the world in 2015.
According to the World Health Organization, more than 90% of COPD deaths are in low- and middle-income countries jar. With increasing smoking rates in developing countries and aging in developed countries, the prevalence of COPD is projected to continue to increase over the next 30 years and by 2030 it is expected to be around 4.5 million people. death from COPD and related diseases. The prevalence is currently highest in the Americas (13.3% in 1990 and 15.2% in 2010) and lowest in Southeast Asia (7.9% in 1990 and 9.7% in 2010).
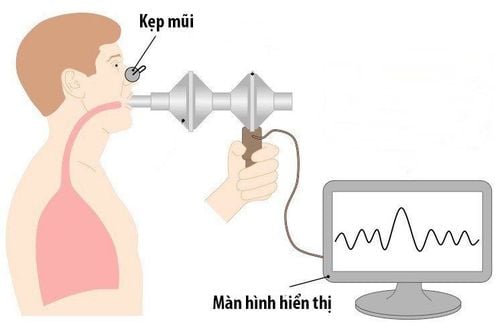
In Vietnam, there are currently no official figures on the prevalence of COPD. According to the epidemiological study on COPD in 2009, the prevalence in adults over 40 years old accounted for 4.2%. Some statistics in the clinical area show that from 1996 to 2000, at Bach Mai Hospital, the rate of patients with COPD entering treatment was 25.1%, ranking first in lung disease. In the two years from 2001-2002, there were 438 COPD patients treated at the Respiratory Department of Bach Mai Hospital. In which, COPD in severe stage (FEV1: 50-30%): 27.1% and very severe stage (FEV1 < 30%): 36.3%[8]. According to GOLD-2019 (Global Initiative for Chronic Obstructive Lung Disease - Global Strategy on COPD), the diagnosis of chronic obstructive pulmonary disease is based on 3 criteria:

Symptoms: Shortness of breath, chronic cough, sputum Exposure to risk factors: Tobacco, occupation, indoor and outdoor pollution. Pulmonary function measurement: FEV1/FVC < 70% after negative bronchial recovery test. Assess the severity of COPD according to GOLD - 2019, divided into 4 groups as follows:
COPD group A - Low risk, few symptoms: 0 - 1 exacerbation in the past 12 months (exacerbation without hospitalization and no antibiotics or corticosteroids) and mMRC 0 - 1 or CAT < 10. COPD group B - Low risk, multiple symptoms: 0 - 1 exacerbation in the past 12 months (non-hospitalized exacerbation, no) must use antibiotics, corticosteroids) and mMRC ≥ 2 or CAT score ≥ 10. COPD group C - High risk, few symptoms: ≥ 2 exacerbations in the past 12 months (or 1 severe exacerbation requiring hospitalization or requiring intubation) and mMRC 0 - 1 or CAT score <10. COPD group D - High risk, multiple symptoms: 2 exacerbations in the past 12 months or 1 exacerbation requiring hospitalization and mMRC ≥ 2 or CAT score ≥ 10. Mechanism of chronic obstructive pulmonary disease:
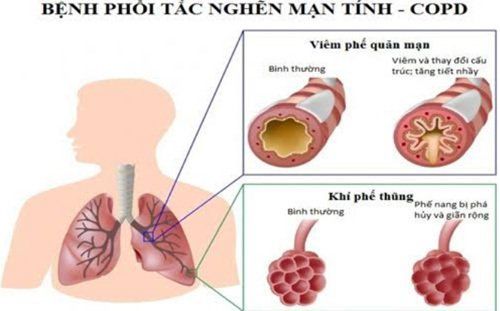
Increased inflammatory response of the airways: A prominent feature of COPD is frequent inflammation, overexpression in the entire airways and lung parenchyma. The inflammatory mediators associated with COPD include: leukotriene B4 (LB4), interleukin 8 (IL-8), IL-1β, IL-6, and tumor necrosis factor-α (TNF-α). These substances amplify the inflammatory process and contribute to the systemic effects of COPD. Several other chemical mediators such as transforming growth factor (TGF) or EGF (epidermal growth factor) are expressed by the growth of epithelial and mucinous cells. The consequences of lung parenchymal injury and increased mucus secretion, airway narrowing, fibrosis, destruction of the lung parenchyma, and changes in the pulmonary capillary bed will lead to decreased airflow and characteristic pathological changes. for COPD.
Proteinase imbalance - Proteinase resistance: Is the pathogenesis of the development of pulmonary emphysema and loss of lung elasticity. In COPD, the balance is tilted towards increased proteolysis due to increased protease. Increased proteases include: serine proteases, polymorphonuclear leukocyte Elastase, Cathepsin G, Proteinase 3, cysteine proteinases, Cathepsin B, K, L, S; Intercellular metalloproteinases (MMPs). Reducing antiprotease includes: alpha-1 antitrypsin, alpha-1 antichymotrypsin, Elafin inhibits leukoprotease secretion, Cystatins.
Mechanism of oxidative - non-oxidative imbalance: Markers of oxidative stress were found in bronchial fluid, in breath and in urine of smokers and patients with COPD. Activation of oxidative status not only damages lung tissue but also participates in protease - non-protease imbalance. Antioxidants also support the inflammatory process such as promoting the activity of genes that produce inflammatory chemical mediators such as IL-8, TNF-α and cause airway narrowing. Experimentally, H2O2, precursor F2α - III causes airway smooth muscle constriction.
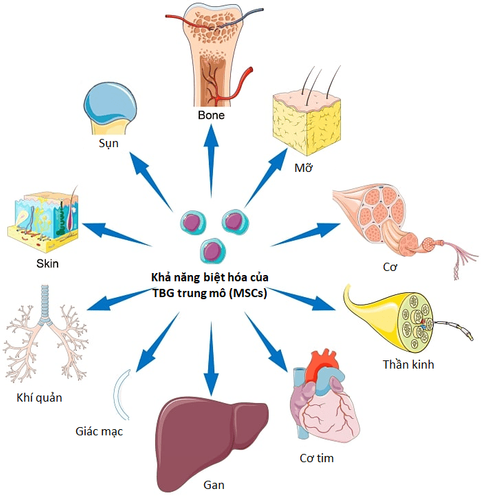
2. Application of Stem Cells in Chronic Obstructive Pulmonary Disease
Many preclinical studies have reported mesenchymal stem cells (TBGTM) to repair damaged lung structure and function in mouse models of COPD. These studies have applied autologous stem cells from bone marrow or stem cells from adipose tissue to treat different animal models of COPD. Although cell dose, frequency, and method of infusion have varied between studies, studies have shown positive results such as decreased inflammation and improved respiratory function weeks or months after stem cell transplantation. .
In 2013, Weiss evaluated the safety and feasibility of stem cell transplantation from bone marrow obtained from healthy donors treated with stage II or III COPD. A total of 62 patients were randomly assigned to 2 groups of disease and control and were followed up for 2 years. Stem cells are introduced into the body through an intravenous route, infused 4 times in 4 consecutive months, observed in the first 2 years without any complications / complications related to stem cell transplantation. There were no significant differences between the number of events (AE) and the frequency of COPD exacerbations in patients receiving TBG transfusion. However, the TBG infusion group observed a decrease in CRP index after stem cell transplantation.
Ribeiro-Paes et al in 2011 conducted a study to evaluate the safety and effectiveness of bone marrow autologous mononuclear stem cell infusion therapy in the treatment of 4 patients with stage IV COPD with middle age. average is 65.8 and all 4 cases are male. Autologous mononuclear stem cells are infused through a peripheral vein. The results after 1 year of follow-up showed that no adverse events were observed, and the quality of life and clinical status of 4 patients also improved markedly. However, after 30 days to 90 days, lung function indices tended to decrease, although not below baseline values before treatment, suggesting that stem cell monotherapy Autologous agents may be beneficial for stimulating long-term lung regeneration.
In 2013, Stessuk used autologous mononuclear stem cells from bone marrow to treat 4 patients with grade III or IV COPD and aerosol monitoring within 3 years after infusion. The results showed that the therapy was safe, without any adverse events. There is an improvement in aerosol measurements, quality of life and slow disease progression after stem cell transplantation.
In 2016, 8 COPD patients over 40 years old were used by Stolk using autologous stem cells from bone marrow with an average infusion dose of 1.5x 106 million cells/kg body weight, 2 times each time 1 week apart. Follow-up results showed that no side effects related to TBG infusion occurred and lung tissue showed no fibrosis response.
In 2018, Zhongwei performed a review of the status of preclinical studies and clinical trials on COPD. Many preclinical studies have shown that exogenous TBG is capable of structural repair and improved respiratory system function in a chronic obstructive pulmonary disease model. Retinoic acid has been shown to regenerate and repair damaged lung structures in COPD mouse models. All three studies using autologous stem cell stem cells from bone marrow showed safety and efficacy in patients with severe and very severe COPD. However, because there was no control group, it could not be concluded whether altering FEV1, weight, lung density and CD31 expression was affected by LVRS and autologous bone marrow stem cell stem cells.
In Vietnam, Van Hanh Hospital initially studied to evaluate the role of stem cells from umbilical cord in the treatment of COPD since 2015. The study design is a clinical trial, phase II, controlled, random, matched pairs. The study was conducted in 2 groups with a group of 10 patients receiving a mixture of autologous stem cells from adipose tissue + platelet-rich plasma and a control group of 10 patients. These patients were all followed up for 6 months and after 6 months, the intervention group received a second infusion of a mixture of autologous stem cells from adipose tissue + platelet-rich plasma. The two groups continued to be followed up to 12 months for clinical and adverse events. Research results are still in the process of acceptance. However, initially, there were no adverse events related to autologous stem cell infusion from adipose tissue.
Bach Mai Hospital in collaboration with the 108 Clinical Research Institute of Medicine and Pharmacy is also carrying out a state-level project to research the use of autologous stem cells from adipose tissue and bone marrow in the treatment of chronic obstructive pulmonary disease. count. The study was conducted on more than 90 patients, divided equally into 3 groups: 30 COPD patients were treated with autologous stem cells from adipose tissue, 30 COPD patients were treated with autologous stem cells from bone marrow, 30 patients with COPD were no intervention as a control group. All patients were followed up for 12 months. The study is currently in progress and is expected to end in October 2019.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.