This is an automatically translated article.
Hepatitis E has traditionally been considered an acute, self-limiting disease similar to hepatitis A. Recently, however, hepatitis E has been identified with the potential to progress to cirrhosis. Chronic hepatitis E occurs mainly in people taking immunosuppressive drugs such as solid organ transplants, HIV infection with low CD4 cell counts, and blood malignancies undergoing chemotherapy.
1. What is Hepatitis E?
Hepatitis E virus (HEV), one of the most common causes of acute hepatitis, affects 20 million people each year and an estimated 3 million symptomatic cases. WHO estimates that hepatitis E caused about 44,000 deaths in 2015 (3.3% of all hepatitis deaths).
According to the study, 4 different HEV genotypes that cause disease in humans have been described. Genotypes 1 and 2 cause disease only in humans, and are transmitted via fecal-oral and waterborne routes. Genotypes 3 and 4 circulate in a number of animals such as pigs, wild boar, deer, and occasionally cause disease in humans.
The virus is shed in the feces of an infected person and enters the human body through the intestinal tract. The hepatitis E virus is transmitted by the fecal-oral route, mainly through contaminated water.
Hepatitis E is usually self-limited and resolves within 2–6 weeks. Sometimes a more serious complication is fulminant hepatitis (acute liver failure) and can be fatal.
Hepatitis E is found worldwide, but is most common in East and South Asia. The disease is prevalent in low- and middle-income countries with limited access to essential water, sanitation and health services. In these areas, hepatitis E can occur in epidemics and in odd cases, mainly caused by contaminated water, mainly caused by genotype 1 virus and a few by genotype 2 virus. cause.
In settings with better sanitation and water supply, hepatitis E infection is infrequent, with occasional odd cases caused by genotype 3 virus, by eating particularly undercooked animal meat. pork and animal liver.

Viêm gan siêu vi e do virus Genotype có thể gây nguy hiểm cho người mắc phải
2. What are the signs and symptoms of hepatitis E?
The incubation period after exposure to HEV ranges from 15-60 days (median 40 days). Most people infected with the hepatitis E virus have no symptoms. When symptoms appear, they are similar to other types of acute viral hepatitis and are usually self-limiting within 4-6 weeks and include:
Mild fever, fatigue Loss of appetite Nausea, vomiting Abdominal pain Liver to Jaundice , dark yellow urine Joint pain Most people with hepatitis E make a full recovery. In rare cases, acute hepatitis E can be severe and lead to acute liver failure. Pregnant women, patients with chronic liver disease, and heavy alcohol consumption are at increased risk of acute liver failure and death. The mortality rate in the presence of exacerbations is about 1%.
Up to 20–25% of pregnant women may die from hepatitis E during the third trimester of pregnancy.
The specific infectious period for HEV is not well defined. But the virus is shed in the stool of an infected person from 1 week before the onset of symptoms until 30 days after the onset of the disease. People with chronic hepatitis E virus infection shed the virus until they are completely cured.
In addition to causing damage to the liver, sometimes HEV can manifest clinically in other organs such as neurological, renal, pancreatic and hematological. Neuropathies associated with HEV include polyneuritis, Guillain-Barré syndrome, facial nerve palsy, ataxia, and psychosis. Thrombocytopenia, marrow hypoplasia, and hemolysis are hematological diseases associated with HEV.
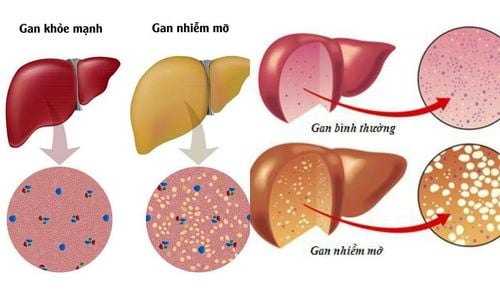
3. Does hepatitis E progress to cirrhosis?
Chronic HEV infection is defined as detection of HEV RNA in patient serum or stool for longer than six months. Similar to other patients with chronic viral hepatitis, symptoms of the disease appear minimal and nonspecific until progression to decompensated cirrhosis.
Hepatitis E can progress to cirrhosis in patients taking immunosuppressive drugs. Immunosuppressed patients include solid organ transplant recipients, HIV-infected and low CD4 T-cell counts, and hematologic malignancies undergoing chemotherapy. After solid organ transplant patients infected with hepatitis E virus have a 50% chance of developing chronic hepatitis E and possibly cirrhosis within a few years.
To date, there have been no reports of progression of acute hepatitis E to cirrhosis in developing countries, where HEV genotypes 1 and 2 are major causes of hepatitis E.
However, on More and more HEV genotype 3 infections acquired in developed countries are progressing to chronic liver disease. These chronic cases occur mainly in solid organ transplant recipients receiving immunosuppressive therapy. Chronic HEV genotype 4 infection has been reported in only a few transplant patients.

Viêm gan siêu vi e có thể khiến người bệnh gặp tình trạng xơ gan trong một thời gian
4. Hepatitis E . test
HEV infection should be considered in any person with symptoms of viral hepatitis, a negative test result for hepatitis A, B, C... and after all have been ruled out. other causes of acute liver injury.
Any patient with symptoms of hepatitis who has traveled to an endemic area or has had an outbreak of hepatitis E should be evaluated for HEV risk. This patient should have a detailed history of travel, drinking water, eating undercooked food, and contact with someone with jaundice to support the diagnosis.
Confirmation of hepatitis E infection is usually by testing for antibodies against HEV or HEV RNA, including the following:
Serum anti-HEV - IgM antibody test: IgM anti -HEV (+) as soon as symptoms appear and for up to 6 months. IgG anti-HEV (+) 10-12 days after the onset of the disease and can persist for many years. HEV RNA in blood or stool Patients with normal immune system:
IgM anti-HEV (-): no evidence of recent HEV infection IgM anti-HEV (+): likelihood of recent HEV infection Current or current Immunosuppressed patient:
IgM anti-HEV (-), additional HEV RNA test: if HEV RNA (+): possibility of HEV infection. Case of HEV RNA (-): no evidence of current or recent HEV infection IgM anti-(+): possibility of recent or current HEV infection In addition, tests to rule out viral pathogens Other hepatitis is also indicated:
IgM antibodies against HAV Hepatitis B surface antigen: HBsAg Antibodies to hepatitis C virus (anti-HCV) and HCV-RNA.
5. Treatment of hepatitis E
Treatment for hepatitis E depends on the patient's immune status and the stage of the disease.
Acute hepatitis E is usually self-limiting without treatment in patients with normal immune systems. Currently, there is no specific antiviral drug therapy for hepatitis E, but mainly supportive treatment, such as: rest, adequate nutrition. don't drink alcohol and avoid drugs that can harm the liver – especially acetaminophen.
Indications for hospitalization in severe cases, acute liver failure and should be considered for pregnant women.
The role of antiretroviral therapy, such as ribavirin, in acute HEV infection in immunosuppressive patients is uncertain.
In patients with chronic HEV infection and taking immunosuppressants, the immunosuppressive drug can be adjusted and the antiviral drug used, such as ribavirin, peginterferon, or a combination of both.
Ribavirin should not be administered to patients who are pregnant and have acute HEV infection due to the risk of teratogenicity.

Vấn đề điều trị viêm gan siêu vi E phụ thuộc vào cơ địa của mỗi bệnh nhân
6. Prevention of Hepatitis E
There is currently no FDA-approved vaccine for hepatitis E. However, in 2012, a vaccine to prevent hepatitis E virus infection was developed and licensed in China, but still not available elsewhere.
Good personal and environmental hygiene are effective approaches to fight hepatitis E virus infection, including:
Do not drink water or ice of unknown purity Do not eat undercooked pork, venison living. Wash hands with soap and water before preparing food and after using the toilet.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.