This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Weight loss surgery, especially Y-Roux bypass, has been shown to be better than conservative and/or medical treatment for weight loss and resolution of obesity-related diseases, but has risks complications of surgery, reoperation and, very rarely, paradoxical progression of nonalcoholic steatohepatitis.
Once liver disease develops in the late stages, obese patients benefit from liver transplantation (LT), but may be at increased risk for perioperative infectious complications. After liver transplantation, metabolic comorbidities are often observed, regardless of underlying liver disease, but patients with fatty liver disease associated with metabolic dysfunction/nonalcoholic steatohepatitis even have a higher risk of disease recurrence. Few studies with low patient numbers have evaluated if and when bariatric surgery may be an option to avoid recurrence, but more high-quality studies are needed to definitively determine. irrespective of the underlying liver disease, but patients with metabolic dysfunction-associated fatty liver disease/nonalcoholic steatohepatitis have an even higher risk of disease recurrence.

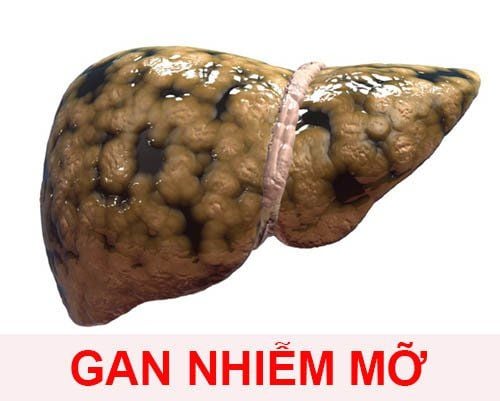
1. Weight loss surgery and fatty liver disease associated with metabolic dysfunction /nonalcoholic steatohepatitis
As mentioned above, the coexistence of several metabolic diseases, summarized as metabolic syndrome, has led to the development of invasive/surgical treatment options. Although bariatric surgery was a niche phenomenon for several years, its benefits in relation to weight loss and improvement in insulin resistance/type 2 diabetes were then established. Furthermore, because of the improved success rates associated with weight loss compared with conservative approaches, patients with bariatric surgery had a significantly better 10-year and 20-year survival compared with those who did not. Equivalent individuals received conservative treatment, despite this improvement, their life expectancy was still lower than that of the general population. Recent evidence suggests that the primary benefit is the result of weight loss and is not attributed to any other metabolic effects of bariatric surgery.
2. Bariatric surgery is not considered the optimal treatment option in nonalcoholic steatohepatitis
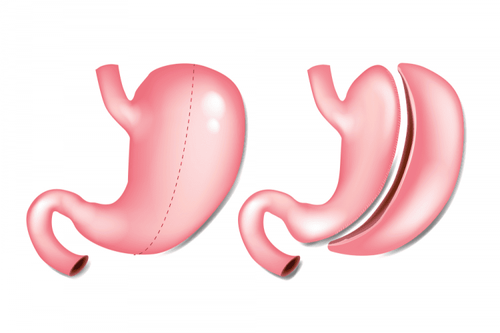
In terms of liver-specific outcomes, bariatric surgery was not considered a treatment option in some meta-analyses of nonalcoholic steatohepatitis remission, despite well-designed studies. suitable. Overall, bariatric surgery resolved nonalcoholic steatohepatitis in the majority of patients (85% in a study by Lassailly et al, with 64.2% of patients undergoing bypass surgery). and 5.5% sleeve gastrectomy) and progressive fibrosis. However, not all procedures are created equal, and Y-Roux bypass surgery is considered the most effective strategy for sustainable weight loss to date.
A recent hierarchical network meta-analysis included 48 high-quality trials and found that pioglitazone and gastric Y-Roux bypass surgery were most effective in improving the liver disease activity score nonalcoholic adiposity, suggesting a causal link between glucose metabolism and fatty liver development.

3. Metabolic disease does not exist as a separate disease but must be treated together
While bariatric surgery affects nonalcoholic steatohepatitis, liver fibrosis, expectedly, also impacts postoperative outcomes after bariatric surgery. This, again, emphasizes that metabolic diseases do not exist as a separate disease but must be treated together. Importantly, bariatric surgery is only performed for patients who are severely obese, while the general population is generally overweight, but not obese, and therefore ineligible for surgery, requiring further studies. Subsequent baseline studies disturb the mechanism of development of fatty liver disease associated with metabolic dysfunction/nonalcoholic steatohepatitis. Notably, a very small fraction of patients develop nonalcoholic steatohepatitis or have worsening nonalcoholic steatohepatitis/fibrosis following bariatric surgery, requiring adequate postoperative care to develop early detection of complications and further emphasizes the need for ongoing research. Given the increasing use of bariatric surgery, prospective studies answering remaining questions about the association of insulin resistance, fatty liver, and fibrosis progression will be available in the near future. .
Conclusion
Bariatric surgery is more effective for weight loss in obese patients than conservative weight loss regimens, however, the risk of bariatric surgery is higher in patients with chronic liver disease and in some patients, severe liver dysfunction after bariatric surgery has occurred.
Statins should be prescribed to all patients with compensated dyslipidemia or other risk factors such as cardiovascular disease, but with excessive use. While there is evidence that statin therapy is safe and also effective in patients with metabolic dysfunction-associated fatty liver disease/nonalcoholic steatohepatitis, large randomized controlled trials still missing. With regard to type 2 diabetes therapy, new anti-hyperglycemic agents such as pioglitazone or GLP-1 agonists show promise, but specific adverse events can be detrimental and must be considered. review.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.