This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
The 2019 worldwide outbreak of coronavirus disease (COVID-19) challenged healthcare system priorities for the clinical management and transmission of various infections, especially those associated with comorbidities of liver disease.
Epidemiological data have demonstrated that COVID-19 patients with altered liver function due to hepatitis infection and cholestasis have a poor prognosis and worse health outcomes. COVID-19-associated liver injury is associated with various liver diseases following severe acute respiratory syndrome-coronavirus type 2 (SARS-CoV-2) infection that may progress during patient treatment COVID-19 with or without pre-existing liver disease.
1. Clinical challenge of COVID-19-associated liver disease
Several studies have addressed clinical challenges. Of relevance is a report by Vespa et al. of an increase in ALP values due to hepatic nutrition of SARS-CoV-2 through the ACE2 receptor on hepatocytes and bile cells. Furthermore, they correlated with increased ALP as a marker of patient frailty or as representative of an increased systemic inflammatory response to SARS-CoV-2 infection. The rate of altered liver injury markers is strongly associated with drug-induced liver injury (DILI) during the COVID-19 pandemic. Some research. A pharmacologically related potential harm with lopinavir/ritonavir has been reported in COVID-19 patients and the patient's vulnerability to the development of severe pneumonia through increased LFTs. Furthermore, pathological features of liver injury through autopsy analysis of COVID-19 patients provide evidence in favor of DILI. One study found moderate microscopic steatosis with mild liver inflammation, suggesting possible liver damage. However, this pattern of histological damage may be correlated with DILI or SARS-CoV-2 infection Several risk factors may be associated with the incidence of liver injury due to COVID-19
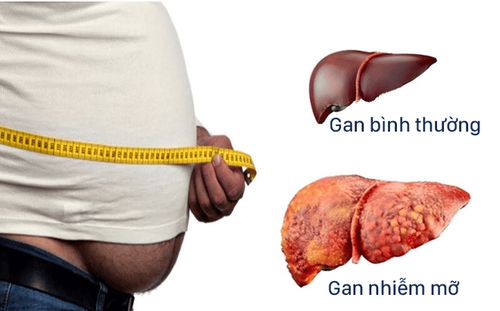
A retrospective study in a French population showing marked obesity rates in confirmed COVID-19 patients. The study included 340 COVID-19 patients, 230 (68%) with non-morbid COVID-19 and 110 (32%) with critical COVID-19. It was found that 85 of the 340 patients with severe COVID-19 (25%) were obese compared with 15.3% of the general French population. After normalizing for age and sex, obesity prevalence was 1.35% and 1.89% higher, respectively, in patients with severe COVID-19 and in those admitted to the care unit. in particular, relative to the general French population. Similarly, Zheng et al. reported a major association of obesity with severity of COVID-19 in patients with metabolic-associated fatty liver disease, which provides the basis for the possibility of the magnitude of the disease. importance of obesity-related liver diseases.
2. Pre-existing chronic liver disease and Covid-19: Relation and Consequences
Chronic liver disease is an existential threat, the leading cause of liver-related death worldwide. Major chronic liver diseases, including hepatitis B or hepatitis C virus infection, alcoholic liver injury (ALD), and NAFLD, lead to persistent liver damage and increased incidence of related cancers associated with chronic liver disease, especially HCC. Underlying liver diseases were one of the key pathogens in the previous SARS outbreak, with high mortality rates among adults and older adults. The Centers for Disease Control and Prevention recently included liver disease as a comorbidity and predisposing factor for SARS-CoV-2 infection. Furthermore, the American Association for the Study of Liver Disease (AASLD) endorses COVID-19 testing on a priority basis for patients presenting with symptoms of liver disease.
The COVID-19 pandemic coupled with the worldwide threat of chronic liver disease further complicates the care of patients with pre-existing liver disease due to lack of testing and monitoring. Therefore, the complex association between pre-existing liver disease and COVID-19 requires further research and disease-specific management. It can be seen that patients with underlying liver diseases are more vulnerable to exacerbation of COVID-19-related and conversely effects that can lead to morbidity and mortality. mortality during the current COVID-19 pandemic.
3. Alcohol use disorder or alcoholic liver damage is the chronic liver disease with the highest burden of hospitalization
Regarding pre-existing liver diseases, alcohol use disorder or alcoholic liver injury is the chronic liver disease with the highest hospitalization burden and has more than doubled in China. This effect is likely to be repeated in the United States, with an estimated 12.7% hospitalization rate associated with COVID-19. The incidence of alcoholic liver injury is increasing with an increase in patients indicated for liver transplantation before the COVID-19 pandemic. The direct clinical impact of COVID-19 on alcoholic liver injury is still unknown, but it can be suspected that SARS-CoV-2 infection may be a major host risk factor with liver injury. primary alcoholic liver injury and subsequent acute-chronic liver failure. The high prevalence of alcoholic liver injury among chronic liver disease patients is reflected in the number of patients with decompensated alcoholic liver injury during the COVID-19 pandemic.
4. Patients with metabolic-associated fatty liver disease are at higher risk of developing COVID-19 disease
Increasing evidence of liver disease comorbidities associated with COVID-19 suggests that patients with metabolic-associated fatty liver disease are at increased risk of developing COVID-19 disease. A retrospective study conducted by Fondevila et al described a mechanistic approach in the context of a higher risk of SARS-CoV-2 infection in obese patients. They evaluated hepatic mRNA expression of the cell-infiltrating molecules SARS-CoV-2, ACE2, and the transmembrane serine 2 protease (TMPRSS2) in obese patients with NAFLD and/or type 2 diabetes. Based on hepatic mRNA expression of both ACE2 and TMPRSS2 in obese patients, the results suggest that SARS-CoV-2 entry factors are differentially affected in diabetes and NAFLD. Furthermore, large changes in the expression of SARS-CoV-2 invading molecules in men and women suggest that women are less susceptible to liver damage. While obese women with diabetes had unexpectedly lower levels of ACE2 and TMPRSS2 than obese women without blood sugar, obese patients with nonalcoholic steatohepatitis had higher expression of those genes, suggesting that advanced stages of NAFLD can lead to COVID-19.5. COVID-19 patients with concomitant advanced liver complications are at higher risk of infection
COVID-19 patients with concomitant advanced liver complications are often at higher risk of infection due to the immune dysfunction associated with cirrhosis. A retrospective study by Iavarone et al noted a significant 30-day mortality rate of 34% in a cohort of 50 cirrhotic patients with COVID-19, a rate higher than the rate in patients with cirrhosis. cirrhosis of the liver with a bacterial infection. Overall COVID-19 mortality from medical consequences of respiratory failure is correlated with worsening of liver dysfunction.
Other types of liver disease COVID-19 patients of great concern are liver transplant recipients and patients with autoimmune liver disease who are taking immunosuppressive drugs. However, the effects related to COVID-19 in living contract donors are still unclear. A case reported by the American Society of Transplantation and the American Society of Transplantation Surgeons described the impact of hepatitis caused by COVID-19 during liver transplantation. A patient underwent a liver transplant from a living donor who was not compatible with ABO without knowing that the donor was infected with COVID-19 during the donation process. In that case, donor-to-recipient transmission was not determined, and the liver donor was found to be recovering from COVID-19 infection. Donor-derived transmission has not been identified.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.