This is an automatically translated article.
Posted by Doctor Nguyen Thi Hoai Nam - Department of Surgical Anesthesia, Vinmec Central Park International General HospitalCurrent data are only sufficient to form a hypothesis that an anesthetic approach to surgery for primary cancer may influence recurrence or metastasis, but a causal link can only be proven by prospective, randomized, clinical trials.
1. Summary
Cancer is a leading cause of morbidity and mortality worldwide and its incidence is increasing. Death is usually due to recurrence or metastasis. Surgical resection of the primary tumor is the mainstay of treatment, but this involves inadvertent dissemination of neoplastic cells into the blood and lymphatic system. The fate of the seeding cells depends on the balance of perioperative factors that promote tumor growth and development (including single surgery, multiple anesthetic agents, acute postoperative pain, and opioid analgesics) along with the patient's perioperative immunological status.
The available evidence from experimental cell cultures and live animal data for these factors is summarized, together with clinical evidence from retrospective studies. Taken together, the current data are only sufficient to form a hypothesis that an anesthetic approach to surgery for primary cancer may influence recurrence or metastasis, but a causal link is only may be demonstrated by prospective, randomized, clinical trials. More research is ongoing, but final results may not be obtained for the next 5 years or so. Meanwhile, there is no solid evidence to support a change in anesthesia in cancer patients, pending the results of ongoing clinical trials.

Một số loại thuốc được sử dụng trong phương pháp phẫu thuật gây mê
2. Make a problem
Despite significant progress in cancer treatment, it remains a major cause of morbidity and mortality. In 2008, 12.7 million new cancer cases were diagnosed worldwide, with 7.6 million cancer-related deaths during that period. In the United States, an estimated 1500 people die from cancer every day, while in the UK more than a third of people will develop some form of cancer during their lifetime. The incidence of cancer continues to increase, therefore, anesthesiologists are faced with the challenge of managing cancer patients with increasing frequency.
In many cancers, extensive surgical resection and resection of the primary tumor are the mainstays of treatment; however, metastatic recurrence is common. Recent recognition suggests that a number of perioperative factors can directly affect cancer cells and also influence cell-mediated immunity, thereby potentially promoting the development of cancer cells. (Table 1)
Here we review the literature on the hypothesis that anesthetic and analgesia methods in primary cancer surgery influence long-term outcomes, explaining the biology of the cells Cancer and perioperative factors may influence metastasis, including available clinical data. The material in this review was obtained from PubMed searches & up to August 2012. Results include all languages.
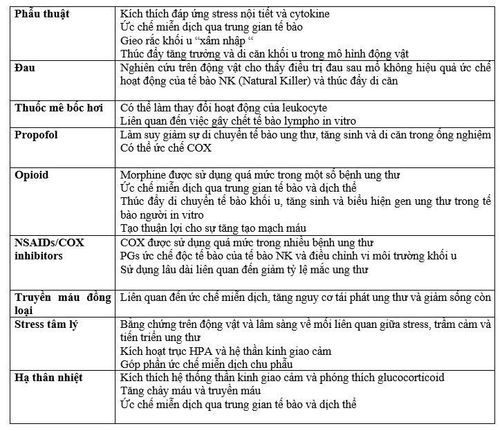
Bảng 1. Các yếu tố chu phẫu có thể ảnh hưởng đến tái phát ung thư và di căn như thế nào?
3. Cancer Cell Biology and Metastasis
Metastasis is a complex process, initiated by detachment of metastatic cells from the primary tumor and finally manifested by tumor proliferation in a distant organ. Establishing an independent blood supply (neoangiogenesis) and evading the host immune barrier are processes necessary for successful tumor growth. The outcome of metastasis depends on a multitude of interactions between the host immune system and the tumor propensity to metastasize. Tumor cells result from a single cell that undergoes many cycles of division and mutation. The mutated cell is "genetically unstable", making it susceptible to additional mutations.
Tumor cells become intractable with normal signaling that regulates cell division and subsequent uncontrolled cell proliferation. Extensive angiogenesis must occur to meet the growing demands of the growing tumor. Furthermore, tumors may not be viable when > 2mm in diameter without vascular neoplasia. Vascular neoplasia is stimulated by the release of pro-angiogenic factors from the tumor, including vascular endothelial growth factor (VEGF) and Prostaglandin E2.
After the establishment of this new capillary network, a subset of cells separates from the primary tumor and invades surrounding tissues. Infiltration of the basement membrane indicates the transition from benign carcinoma in situ to invasive malignancy. Cancer cells enter the circulatory system by penetrating thin vessel walls, including lymph. The majority of invasive cancer cells are destroyed by the immune system, with 0.1% of cells able to survive 24 hours. A specialized group of macrophages, CD11b+, recognize metastatic breast cancer cells and support their progression. Surviving cancer cells migrate to the capillary bed of a distant organ where they continue to proliferate in the vessel wall and then in the organ's parenchyma.
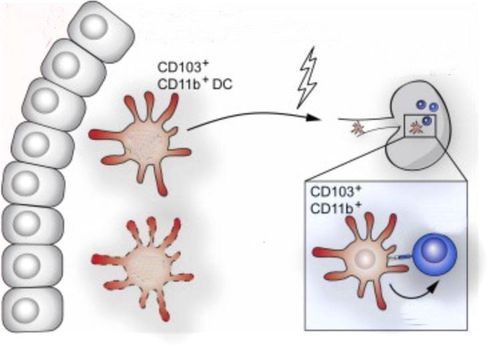
Hình ảnh một nhóm đại thực bào chuyên biệt cùng với CD11b +
4. Cancer and the immune system
Cell mediated immunity constitutes the main defense against invasion by tumor cells and its main components include natural killer (NK) cells, cytotoxic T cells, monocytes and dendritic cells. NKs are large, cytotoxic granulosa lymphocytes that spontaneously recognize tumor cells, without prior sensitization, and induce lysis. There is an association between reduced stress-induced NK cell activity and promotion of breast tumor growth and metastasis in mice and patients with low NK cell counts with an increased risk of developing cancer, or metastasis. post-cancer surgery. Despite intact immunity, some tumor cells evade the host's defenses and continue to grow. The inflammatory state caused by the growing tumor favors the conduction of more immune cells into its 'microenvironment'. The added immune cells may not exhibit the normal protective response leading to tumor cell elimination.
The release of proinflammatory cytokines by these immune cells and by the tumor itself may help balance tumor progression. The immune system is regulated by a variety of cytokines, some of which are implicated in promoting cancer, while others are resistant. Engaging the immune system to induce an enhanced anti-tumor response can be used as an adjuvant cancer therapy. For example, recombinant NK T cells offer therapeutic potential. Promising survival benefit was observed when rats were treated with perioperative 'immunostimulation'.
Composition according to A ́. Heaney1 and D. J. Buggy, “Can anaesthetic and analgesic techniques affect cancer recurrence or metastasis?”, British Journal of Anaesthesia 109 (S1): i17–i28 (2012) doi:10.1093/bja/aes421