This is an automatically translated article.
The article was professionally consulted by Specialist Doctor II Dinh Van Loc - Department of General Surgery - Vinmec Danang International General Hospital. Dr. Loc has advanced training in Anesthesiology and has more than 23 years of experience in anesthesia.Children who are indicated for thoracic surgery, ENT surgery, major surgery, high risk, ... will be assigned endotracheal anesthesia. Anesthesia for tracheal intubation in young children should be performed carefully and in accordance with the correct procedure in order to minimize the risk of complications and ensure the success of surgery.
1. Indications/contraindications for anesthesia for intubation in young children
1.1 Designation
Ear - nose - throat and tooth - jaw - face surgery; Thoracic surgery: Heart, lungs; Surgery requiring the use of muscle relaxants such as abdominal surgery, intestinal volvulus, intestinal obstruction, peritonitis; Major surgery, heavy blood loss and shock; Surgery with an unfavorable position such as the baby lying on the stomach, side or sitting; Surgery requires airway control; Surgery in children at risk of reflux; Surgery involves damage to the lungs and many other organs.
1.2 Contraindications
The operator is not technically proficient; No means of artificial respiration; Children with acute respiratory infections.2. Preparation for endotracheal anesthesia in children
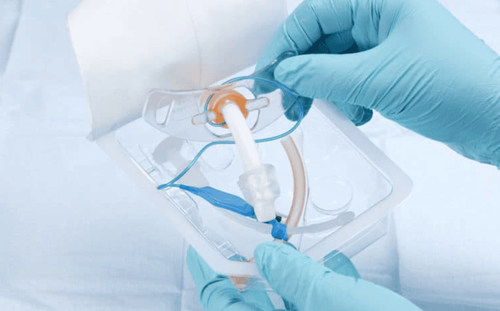
Performer: Anesthesiologist and assistant; Equipment: Anesthesia machine, oxygen, suction machine, catheter, sphygmomanometer, vital indicators monitor, ambu ball, canule mayo, mask, laryngoscope, bronchospasm sprayer, Xylocaine nebulizer, endotracheal tube of appropriate size for the child (the diameter of the tube is equal to the diameter of the child's nostril or the diameter of the tip of the child's little finger); Drugs: Pre-anesthetic drugs with doses calculated according to the child's weight; Seduxen, Midazolam, Atropin in appropriate doses;
3. The process of anesthesia intubation in young children
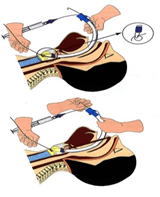
Step 1: Induction of anesthesia and intubationChildren usually initiate anesthesia with a respiratory anesthetic such as sevorane Intravenous induction, using one of the drugs Ketamine, Thiopental or Propofol with appropriate doses; Apply 100% oxygen squeeze ball mask to pediatric patients; For children using muscle relaxants: Use one of the drugs Suxamethonium, rocuronium, vecuronium or Atracurium with appropriate dosage; Intubation for pediatric patients: is a delicate and very gentle operation, otherwise it will cause trauma and edema of the larynx. Hold the laryngoscope, insert the blade into the child's oral cavity; Then, holding the endotracheal tube, insert the tip of the tube through the opening of the vocal cords into the trachea. Next, remove the laryngoscope, inflate the endotracheal tube if present, attach the respiratory system to the oxygen balloon, and examine the chest and abdomen. Finally, secure the endotracheal tube using adhesive tape.
Ensure the following factors: Anesthesia, analgesia, muscle relaxation, vital functions by adjusting the drugs and anesthetic system accordingly; Maintain anesthesia with inhalational or intravenous anesthetics and analgesics and muscle relaxants. Step 3: Resuscitation, extubation
Only extubate when the child fully meets the following conditions:
Self-breathe is good in both amplitude and frequency; (the effect of morphine is over) Only the minimum SpO2 must reach over 96% when ventilation with oxygen support; Children perform the correct movements as required: Open eyes, open mouth, stick out tongue, shake head, lift head off the table,.( End of muscle relaxant effect: TOF≥ 90%
4. Risk of complications and measures to deal with it
Apnea, asphyxiation: It can be caused by high concentration anesthetic injection, rapid injection or by muscle relaxant but not timely artificial respiration. Treatment measures are close monitoring when injecting anesthesia, respiratory support and timely command respiration; Bronchospasm : Manage by giving the child antispasmodics (Salbutamol nasopharyngeal or endotracheal tube) or artificial respiration with an ambu balloon with oxygen mask or endotracheal intubation. ; Laryngeal spasm: The appropriate intervention is to apply a high-pressure oxygen balloon mask to the child. At the same time, let the child sleep more deeply, use muscle relaxants, give artificial respiration until the muscle relaxant runs out, and the child breathes well on his own. If necessary, intubation and artificial respiration can be performed; Vomiting causes reflux: The way to prevent it is to insert a gastric suction tube in the child before anesthesia. If the child has reflux, it is necessary to aspirate the bronchi with 0.9% saline serum, give the child antibiotics, high-dose corticosteroids, oxygen therapy and mechanical ventilation if necessary;
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
SEE MORE
What to know when intubation in children How to intubate emergency? Artificial ventilation for patients with acute pulmonary edema